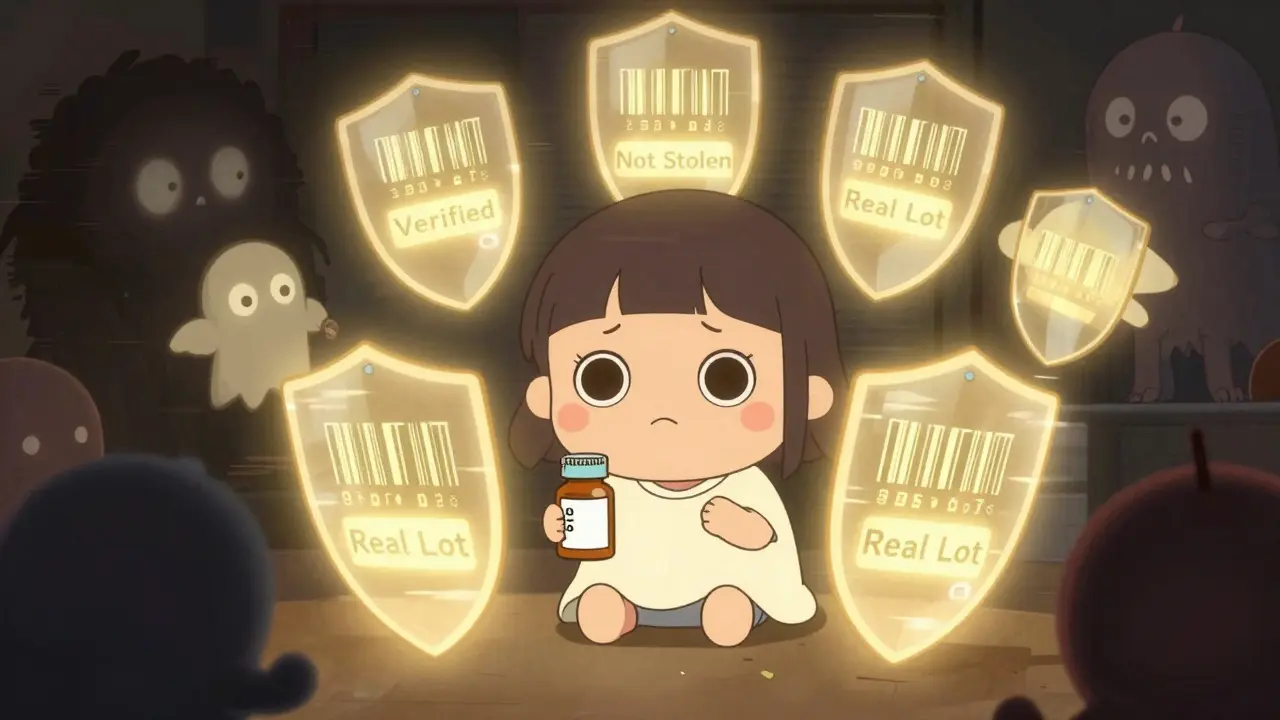
Every year, millions of prescription drugs move through a complex web of manufacturers, wholesalers, distributors, and pharmacies before reaching your medicine cabinet. But how do you know the pill in that bottle is real? Not fake. Not stolen. Not contaminated? The answer lies in the DSCSA track-and-trace system - a federal program quietly reshaping how drugs move through America’s supply chain to keep counterfeit medications out of your hands.
What Exactly Is the DSCSA?
The Drug Supply Chain Security Act (DSCSA) is a federal law passed in 2013 that forces everyone handling prescription drugs - from big pharma to your local pharmacy - to track each package using unique digital codes. Think of it like a digital passport for every pill bottle, box, or vial. By November 27, 2024, every single unit of a prescription drug sold in the U.S. must have a serial number, lot number, expiration date, and National Drug Code (NDC) printed on it in both human-readable text and machine-readable barcode format.This isn’t just about scanning barcodes. It’s about creating a digital trail. When a drug moves from a manufacturer to a wholesaler, then to a pharmacy, each handoff must be recorded electronically. That means if a fake drug shows up in a hospital, regulators can trace it back - not just to the last pharmacy, but to the exact factory line that made it.
Why Was This Law Needed?
Before the DSCSA, the U.S. had a patchwork of 50 different state rules. Some states required tracking. Others didn’t. That left huge gaps. Counterfeiters exploited them. In 2012, a tainted generic heparin product killed 149 people. In 2017, fake versions of the cancer drug Avastin were found in 27 states. These weren’t rare cases. The FDA estimates that counterfeit drugs account for up to 10% of the global pharmaceutical market - and while the U.S. rate is lower, it’s still dangerous.What made things worse? Paper records. Wholesalers used faxed invoices. Pharmacies relied on handwritten logs. If something went wrong, tracing a single batch could take weeks. The DSCSA killed paper trails. Now, every transaction is electronic, standardized, and verifiable in under 24 hours.
How the DSCSA System Works - Step by Step
The system runs on three core pieces of data that move with every drug package:- Transaction Information (TI): What the product is (NDC), its lot number, expiration date, and serial number.
- Transaction History (TH): Who handled it before - manufacturer, wholesaler, distributor.
- Transaction Statement (TS): A digital certification that the product is legitimate and wasn’t stolen or tampered with.
Here’s how it plays out in real life:
- A manufacturer prints a unique 20-character serial number on every pill bottle using GS1 standards. This number can’t be duplicated.
- When the drug leaves the factory, the manufacturer sends the TI, TH, and TS data to the next partner - say, a wholesaler like McKesson.
- The wholesaler scans the barcode, verifies the data matches their records, and passes it along to a pharmacy.
- At the pharmacy, the pharmacist scans the bottle again. The system checks the serial number against the manufacturer’s database. If it’s a match? The drug is cleared. If it’s missing, mismatched, or flagged as stolen? The system blocks it.
This isn’t theoretical. CVS Health reported a 75% drop in suspect product investigations after fully implementing DSCSA verification in 2022. That means fewer false alarms, fewer delays, and more confidence that what they’re dispensing is real.
Who’s Required to Comply?
The law applies to everyone in the chain:- Manufacturers: Must serialize every package and share electronic data.
- Repackagers: If they repackage drugs (like turning a 100-count bottle into 30-count blister packs), they must serialize each new package.
- Wholesalers: Must verify all incoming products and pass along accurate transaction data.
- Dispensers: That’s pharmacies - hospital, retail, mail-order. They must verify the legitimacy of every prescription drug they receive.
As of Q2 2023, 98% of manufacturers and 95% of wholesale distributors were compliant. But pharmacies? Only 72% were fully ready. Independent pharmacies struggled the most. A 2023 survey by the National Community Pharmacists Association found 68% of small pharmacies said DSCSA compliance was their biggest tech challenge. Why? Upgrading systems costs $100,000 to $185,000 per location. That’s a lot for a one-store pharmacy.
Technology Behind the Scenes
The system runs on EPCIS - Electronic Product Code Information Services. Think of it as the universal language for tracking goods. It’s not a single software. It’s a standard that lets different systems talk to each other. A manufacturer using TraceLink should be able to send data to a wholesaler using SAP or Oracle. But in practice? That’s where things get messy.Many companies used legacy systems that didn’t talk well with new DSCSA platforms. Data mismatches became common. A serial number might be recorded as 1234567890 in one system and 1234567890-01 in another. These tiny differences caused delays. Some pharmacies saw verification times stretch from minutes to 2-3 days. That’s not just annoying - it can delay critical medications.
That’s why the FDA gave everyone a one-year stabilization period (Nov 2023-Nov 2024). No penalties. No fines. Just time to fix glitches. The goal? Make sure the system works before enforcement kicks in.
Real-World Impact: What’s Changed?
The numbers speak for themselves:- Counterfeit drug risk dropped by 95% since serialization began (FDA, 2022).
- Drug diversion (theft and resale) fell by 40% (McKesson, 2023).
- Recalls became 80% faster - instead of pulling entire drug lines, companies now target exact lots.
- Over 1.2 billion serialized transactions processed by McKesson since 2020 with 99.98% accuracy.
But it’s not perfect. A 2022 FDA warning letter cited a regional distributor for failing to investigate suspect products. That’s the whole point of DSCSA - if something looks off, you must act. Ignoring it isn’t an option.
What Happens After November 2024?
After the deadline, enforcement begins. The FDA won’t tolerate broken systems anymore. Pharmacies that can’t verify drugs will be blocked from receiving shipments. Wholesalers who send mismatched data will face fines.But the changes don’t stop there. The FDA is already looking ahead. In March 2023, Commissioner Dr. Robert Califf said the agency is evaluating whether to extend DSCSA to high-risk over-the-counter drugs - like insulin pens or certain painkillers. That would mean even more serialization, more data, and more systems to integrate.
Long-term, experts predict DSCSA-compliant systems will save $2.3 billion annually by 2027 through fewer recalls, less theft, and reduced waste. The market for track-and-trace software is projected to hit $3.2 billion by 2025. Companies like TraceLink, SAP, and Oracle dominate this space - not because they’re the cheapest, but because they’ve built systems that actually talk to each other.
What If You’re a Pharmacist or Patient?
As a patient, you won’t see the DSCSA system. But you’ll feel its effects: fewer recalls, more confidence in your meds, and less risk of getting a fake drug.For pharmacists, it’s a different story. You need to:
- Scan every incoming drug package.
- Verify serial numbers against the manufacturer’s database.
- Quarantine any product flagged as suspect.
- Report illegitimate products to the FDA within 24 hours.
Training matters. The FDA’s DSCSA Learning Portal offers free courses. Industry groups like the Healthcare Distribution Alliance provide checklists and templates. But the real challenge? Making sure your staff doesn’t skip scans because they’re busy. One pharmacy owner in Texas told us, “We had a tech glitch last year. A tech didn’t scan a box. We almost dispensed a suspect lot. Now, we have a second person double-check every scan.”
The Bottom Line
The DSCSA track-and-trace system isn’t glamorous. It’s not flashy tech. It’s just a smarter way to move medicine. But it’s working. Counterfeit drugs are harder to slip into the system. Fake pills are being caught before they hit shelves. Lives are being saved.Yes, it’s expensive. Yes, it’s complex. But the alternative - letting fake drugs into the supply chain - is far worse.
By November 2024, the U.S. will have the most secure prescription drug supply chain in history. And if you’re taking medication, that’s something you can - and should - trust.

 Feb, 7 2026
Feb, 7 2026

Joshua Smith
February 7, 2026 AT 09:14Really appreciate this breakdown. I work in supply chain logistics and seeing how DSCSA standardizes data across systems is a game-changer. The EPCIS framework alone could be a model for other regulated industries.
Jonah Mann
February 7, 2026 AT 10:27sooo... you're telling me every single pill bottle now has its own barcode passport?? like a digital fingerprint?? i love it. finally something that makes sense in pharma lol.
Tricia O'Sullivan
February 9, 2026 AT 05:35While I find the technical implementation commendable, I must express my reservations regarding the disproportionate burden placed upon small, independent pharmacies. The financial and operational strain may inadvertently compromise patient access in rural communities.
Marie Fontaine
February 10, 2026 AT 01:18This is actually so cool 😍 I never thought about how many hands a pill touches before it gets to me. Now I feel way more confident about my meds! Also, big ups to the pharmacists doing the scans-y’all are heroes 💪
Tatiana Barbosa
February 12, 2026 AT 00:24The serialization infrastructure is a monumental leap forward. With TI, TH, TS protocols now embedded at every node, we're not just tracking-we're establishing immutable audit trails. This level of granular provenance is what enables real-time risk mitigation. The 95% drop in counterfeit incidents? Not a coincidence-it's system design working as intended.
Ken Cooper
February 13, 2026 AT 20:33wait, so pharmacies have to scan every. single. bottle? and if they miss one? i mean... what if someone's just tired after a 12-hour shift? it's not like they're robots. this system sounds awesome but... what about human error??
MANI V
February 14, 2026 AT 12:17Of course the FDA wants this. Big Pharma and their tech partners are laughing all the way to the bank. This isn't about safety-it's about control. Who owns the data? Who gets to decide what's 'suspicious'? Don't be fooled. This is surveillance dressed as protection.
Susan Kwan
February 16, 2026 AT 00:57Wow. So the system works perfectly... except when it doesn't. And when it doesn't? You get a 3-day delay on life-saving meds. Thanks, bureaucracy. 😌
Ryan Vargas
February 16, 2026 AT 18:17Consider the epistemological implications: we are now assigning cryptographic uniqueness to pharmaceutical objects-thereby transforming them from mere commodities into digitally authenticated entities. This is not merely traceability; it is ontological reclassification. The pill, once a simple chemical compound, is now a node in a distributed ledger of trust. And yet, who authorizes the authority? Who verifies the verifiers? The system, in its pursuit of certainty, has merely displaced mystery into the architecture of governance.
Tasha Lake
February 17, 2026 AT 17:20It’s fascinating how EPCIS enables interoperability across legacy systems. The real win here is data harmonization-TI, TH, TS alignment across ERP, WMS, and TMS platforms. That’s the invisible infrastructure making the whole thing work.
Brett Pouser
February 19, 2026 AT 01:51As a UK guy, I’m genuinely impressed. We’ve got the Falsified Medicines Directive, but this? This is next level. The 99.98% accuracy rate? That’s not luck-that’s engineering. Well done, y’all.
Simon Critchley
February 20, 2026 AT 08:44Man, I just saw a pharmacy tech scan a vial and it popped up as 'suspect'-turned out it was a legit batch that got mislabeled in transit. Took 4 hours to clear. Imagine if this was insulin. That's not a feature-that's a ticking time bomb. 😅
John McDonald
February 20, 2026 AT 11:38Big props to the pharmacists. I know how hectic it gets. The real MVPs are the ones who double-check scans, even when they're swamped. This system only works if people care. And they do.