Head Injury & Urinary Retention Risk Estimator
Select the type of head injury and the affected brain area to estimate the risk of urinary retention:
Ever wondered why a blow to the head can make it hard to pee? It’s not just a coincidence - the brain and bladder are tightly linked through nerves and control centers. When a head injury any trauma that damages the skull or brain tissue, ranging from mild concussions to severe traumatic brain injuries disrupts the signals that tell your bladder when to fill and when to empty, you may end up with urinary retention.
Quick Takeaways
- head injury urinary retention occurs when nerve pathways between the brain and bladder are damaged.
- Severe injuries like traumatic brain injury a disruption of normal brain function caused by external force, often leading to swelling or bleeding have the highest risk.
- Even mild concussion a temporary loss of brain function after a head impact, without structural damage can trigger urinary problems if the autonomic nervous system is affected.
- Symptoms include a weak urine stream, feeling of incomplete emptying, or complete inability to urinate.
- Early evaluation with a urodynamic study a set of tests that measure bladder pressure, flow, and nerve activity can pinpoint the cause and guide treatment.
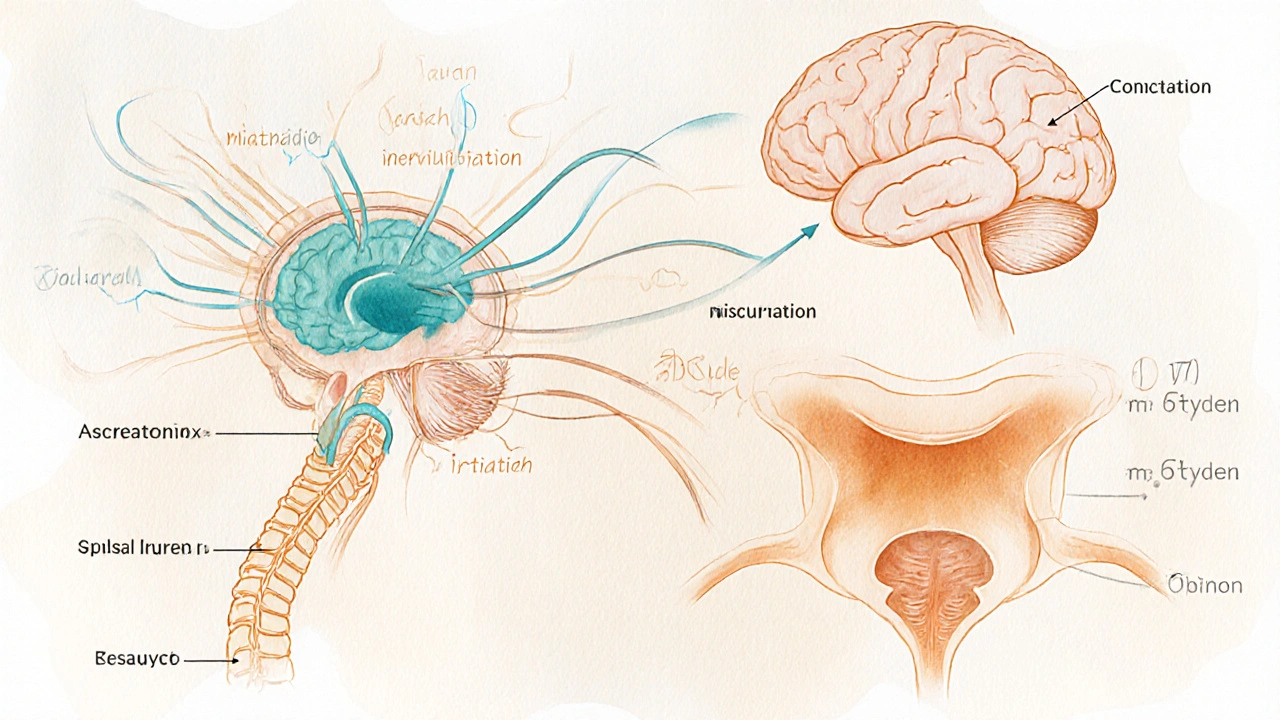
Why the Brain Controls the Bladder
The bladder isn’t a stand‑alone organ; it’s part of a complex communication loop called the micturition reflex the coordinated process where the brain, spinal cord, and peripheral nerves regulate urination. At the top of this loop sit two brain regions:
- Pons (pontine micturition center) - sends the “go” signal to relax the sphincter and contract the bladder.
- Prefrontal cortex - decides when it’s socially appropriate to void.
Both areas rely on the autonomic nervous system the part of the nervous system that controls involuntary functions like heart rate, digestion, and bladder activity. Damage to any of these structures can interrupt the flow of information, causing the bladder to either overfill or fail to contract - the hallmark of urinary retention.
Types of Head Injuries and Their Urinary Risks
| Injury Type | Typical Brain Areas Affected | Retention Risk (%) | Common Urinary Pattern |
|---|---|---|---|
| Concussion | Diffuse axonal stress, minor cortical disruption | 5‑10 | Intermittent hesitancy, occasional overflow |
| Contusion / Hematoma | Pons, basal ganglia | 15‑30 | Reduced stream, sense of incomplete emptying |
| Traumatic Brain Injury (moderate‑severe) | Brainstem, frontal lobes, spinal‑cervical junction | 35‑60 | Complete retention, need for catheter |
| Diffuse Axonal Injury | White‑matter tracts linking brainstem to cortex | 25‑45 | Variable, often progressive |
| Skull Fracture with CSF leak | Basal skull, meninges | 10‑15 | Transient retention, improves with healing |
These numbers come from pooled data in neurology‑urology cross‑sectional studies (e.g., a 2023 multicenter review of 1,200 patients). The trend is clear: the more the brainstem and autonomic centers are involved, the higher the chance of urinary retention.
Spotting the Red Flags
After a head injury, keep an eye on the following signs:
- Difficulty starting a stream or a very weak stream.
- Feeling of a constantly full bladder despite recent voiding.
- Lower abdominal pain or swelling.
- Fever, which could indicate a urinary tract infection caused by retained urine.
- Changes in mental status that make it hard to report symptoms.
If any of these appear within days to weeks post‑injury, it’s time to get evaluated. Ignoring retention can lead to bladder stretching, kidney damage, or chronic infections.
How Doctors Diagnose the Problem
The evaluation usually follows a two‑step approach:
- Neurological assessment: A neurologist checks reflexes, motor strength, and cognition. They specifically test the spinal‑cervical junction the region where the brainstem meets the spinal cord, crucial for autonomic control because lesions there often cause neurogenic bladder.
- Urologic work‑up: This starts with a simple post‑void residual (PVR) scan. If PVR > 150ml, the physician orders a urodynamic study a series of measurements that assess bladder pressure, flow rate, and sphincter coordination. The study can differentiate between an obstructive cause (like prostate enlargement) and a neurogenic cause.
Additional tests may include MRI of the brainstem, cystoscopy, or EMG of the pelvic floor muscles.
Treatment Pathways
Management aims to relieve the retention, protect the kidneys, and restore as much normal bladder function as possible.
Short‑Term Relief
- Intermittent catheterization: A clean‑tech catheter is inserted several times a day to empty the bladder. It reduces infection risk compared to indwelling catheters.
- Alpha‑blockers: Meds like tamsulosin relax the bladder neck, allowing easier flow when partial nerve function remains.
Rehabilitation Strategies
- Pelvic floor physical therapy: Targeted exercises improve sphincter coordination and can boost residual nerve signaling.
- Neuromodulation: Sacral nerve stimulation has shown success in chronic neurogenic urinary retention after traumatic injury.
Long‑Term Options
- Bladder augmentation: Surgical enlargement of the bladder using intestinal tissue can accommodate larger volumes when the bladder can’t contract.
- Permanent catheter or suprapubic tube: Considered when nerve recovery is unlikely after severe brainstem damage.
Each plan is individualized based on injury severity, age, and functional goals. A multidisciplinary team-neurologist, urologist, physical therapist-delivers the best outcomes.
Prevention and When to Seek Help
While you can’t always prevent a head injury, you can reduce its impact:
- Wear helmets for sports, biking, and certain occupations.
- Address concussion symptoms promptly; rest and medical clearance before returning to activity.
- Monitor urinary habits after any head trauma-don’t assume “it’ll pass”.
If you notice any retention signs within the first 48hours or a gradual worsening over weeks, call your healthcare provider. Early intervention cuts the risk of permanent bladder damage.

Frequently Asked Questions
Can a mild concussion cause urinary retention?
Yes, though it’s less common. A concussion can temporarily disrupt the autonomic pathways that regulate bladder emptying, leading to occasional hesitancy or mild retention. Symptoms typically resolve within a couple of weeks, but persistent issues merit a check‑up.
What is the difference between neurogenic bladder and urinary retention?
Neurogenic bladder describes any bladder dysfunction caused by nerve damage - it can lead to over‑activity, under‑activity, or retention. Urinary retention is the specific result when the bladder cannot empty fully, often a subtype of neurogenic bladder.
Do medications for head injury increase the risk of retention?
Some sedatives, anticholinergics, or opioids used for pain and agitation can suppress bladder contractions, worsening retention. Doctors usually balance pain control with the lowest effective dose and consider alternatives when urinary issues arise.
How long does catheter use last after a brain injury?
It varies. For mild injuries, intermittent catheterization may be needed for a few weeks until nerve pathways recover. In severe brainstem damage, long‑term catheterization or a suprapubic tube might be required indefinitely.
Can bladder training help after a head injury?
Bladder training can be effective if some voluntary control remains. A schedule of timed voiding, combined with pelvic floor exercises, helps retrain the residual nerves and can reduce reliance on catheters.

 Sep, 30 2025
Sep, 30 2025
diego suarez
September 30, 2025 AT 20:28Thanks for pulling together all that information. It’s good to see the link between the pons and bladder control laid out clearly. For anyone dealing with a concussion, keeping an eye on urinary habits can catch a problem early. A simple post‑void residual scan is often enough to decide if further testing is needed.
stephen henson
October 11, 2025 AT 06:28Great summary! 👍 The interactive risk estimator is a handy tool, especially for patients who want a quick idea of what they’re facing. Remember, if you’re in the 15‑30% range, it’s worth chatting with a urologist sooner rather than later. Stay safe out there! 😊
Manno Colburn
October 20, 2025 AT 12:41The relationship between head trauma and bladder function is more intricate than most people give it credit for. When the pontine micturition center takes a hit, the whole cascade can go haywire, leading to a spectrum of urinary disturbances. In my experience, even a ‘mild’ concussion can trigger subtle detrusor under‑activity that only shows up on a post‑void residual study. The brain’s autonomic pathways are like a tightrope; a small misstep can cause a ripple that reaches the bladder weeks later. That’s why clinicians should keep a low threshold for ordering a urodynamic work‑up after any significant head injury. A 5‑10% risk isn’t negligible when you factor in the potential for kidney damage down the line. Moreover, patients often dismiss early hesitancy as ‘just holding it in’, which can mask the true underlying neurogenic process. Early intervention with intermittent catheterization can prevent infections and preserve renal function. Pharmacologic agents such as alpha‑blockers may help if there’s residual sphincter tone, but they’re not a cure‑all. Rehabilitation, including pelvic floor therapy, should be introduced once the acute phase clears, because neuroplasticity can aid in regaining some bladder control. For severe TBI cases, sacral neuromodulation has shown promise, though it requires careful patient selection. It’s also worth mentioning that some analgesics and anti‑emetics used post‑injury can exacerbate retention, so medication reviews are essential. In short, the key is vigilance – monitor voiding patterns, use objective measurements, and intervene before complications arise.
Namrata Thakur
October 28, 2025 AT 14:08This article really hits the nail on the head – the brain‑bladder connection is often overlooked until things go south. I’ve seen patients with mild head trauma develop a “full‑bladder” feeling that won’t go away, and the key was early urodynamic testing. Simple interventions like timed voiding and pelvic floor exercises can make a huge difference, especially when the injury is limited to the pons. Don’t wait for a painful urinary infection to force you into a catheter.
Chloe Ingham
November 4, 2025 AT 12:48So they want us to think a simple bump can’t mess with our pee, huh? That’s exactly what the “big pharma” agenda wants – keep us clueless while they push new drugs that hide the real symptoms. Keep your eyes open and don’t swallow every medical press release.
Rhys Black
November 10, 2025 AT 07:41It is a grave societal failing when the medical community glosses over the neurogenic consequences of head trauma. One must demand comprehensive neuro‑urological assessments as a standard of care, not an afterthought. Ignoring the autonomic fallout is tantamount to negligence.
Jaylynn Bachant
November 14, 2025 AT 22:48life is a river flowin thru brain and bladder, when the dam breakin the head it messes up the stream. we gotta listen to our bodies, not just the docs.
Anuj Ariyo
November 18, 2025 AT 10:08Interesting read, really well‑structured; the tables make the data clear, and the step‑by‑step diagnostic flow is helpful. I think anyone who’s had a head knock would benefit from checking the red‑flag list.
Tom Lane
November 20, 2025 AT 17:41Appreciate the balanced view on short‑term versus long‑term solutions. It’s important to tailor catheter decisions to the individual’s recovery trajectory.
Darlene Young
November 21, 2025 AT 21:28Jaylynn, while the poetic vibe is noted, the science here is straightforward – we need objective testing, not mystic metaphors. Early urodynamics can differentiate true neurogenic retention from functional hesitancy, and that’s what saves kidneys.
Steve Kazandjian
November 22, 2025 AT 11:21Bottom line: watch your bladder after any head injury.