Joint Health Massage Guide
Recommended Massage Approach
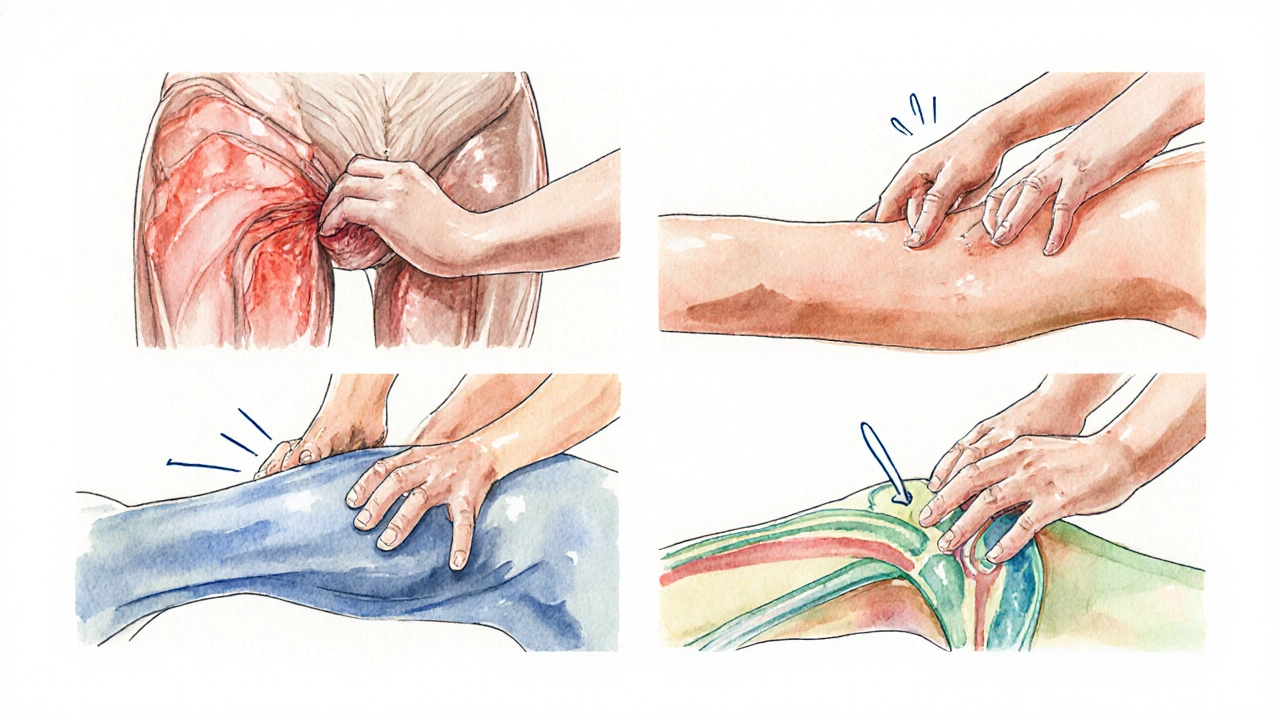
When joints start to ache, swell, or feel stiff, the first thought is often medication or surgery. But massage therapy is a hands‑on treatment that manipulates soft tissue to ease pain, improve circulation, and support healing. Below we break down why this old‑school practice matters for anyone dealing with joint damage, from a runner’s knee to arthritis flare‑ups.
What Massage Therapy Actually Does to Your Joints
Massage isn’t just a luxury; it triggers a cascade of physiological responses:
- Increased blood flow delivers oxygen and nutrients to damaged cartilage and synovial fluid.
- Mechanical pressure reduces inflammationthe swelling response that limits joint mobility by encouraging lymphatic drainage.
- Stretching of surrounding muscles restores range of motionthe degree to which a joint can move without pain and lessens stress on the joint surface.
- The nervous system releases endorphinsnatural pain‑relieving chemicals that also improve mood, lowering the perception of pain.
These effects work hand‑in‑hand with conventional rehab tools, making massage a valuable ally in joint recovery.
Key Joint Conditions that Benefit from Massage
Not all joint problems are the same, but many share common pain pathways that massage can target.
- Osteoarthritisdegenerative wear‑and‑tear of cartilage, often in knees, hips, and hands - massage improves synovial fluid circulation, easing stiffness.
- Rheumatoid arthritisautoimmune inflammation that attacks joint linings - gentle techniques calm inflammatory mediators.
- Sports injuriessprains, strains, and micro‑tears around joints - deep‑tissue work accelerates tissue repair.
- Post‑surgical scar tissuefibrous buildup that restricts joint movement - myofascial release softens adhesions.
Even chronic conditions like chronic low back pain or hip bursitis see measurable improvements after a regular massage schedule.
Massage Techniques That Target Joint Health
Different strokes serve different needs. Here’s a quick rundown of the most joint‑friendly styles:
- Myofascial release - slow, sustained pressure on the fascia (the connective tissue envelope). It frees trapped fibers that pull on joints.
- Trigger point therapy - focused pressure on hyper‑irritable spots in muscle. Relieving these knots reduces referred pain that often disguises itself as joint ache.
- Swedish massage - long, gliding strokes that boost circulation without over‑loading sensitive tissues.
- Deep‑tissue massage - firmer pressure for athletes or people with thick muscle layers; best used after inflammation subsides.
- Joint mobilization - therapist‑guided passive movements that gently stretch the joint capsule and improve synovial flow.
Choosing the right method depends on the stage of injury. Early inflammation calls for light, Swedish or lymphatic massage; later phases can handle deeper myofascial work.
Integrating Massage with Physical Therapy and Rehab
Think of massage as a bridge between passive healing and active rehab. A typical week might look like this:
- Day 1‑3: Light Swedish massage to reduce swelling and promote circulation.
- Day 4‑7: Begin gentle range‑of‑motion exercises prescribed by a physical therapista licensed professional who designs movement‑based recovery plans.
- Day 8‑14: Add myofascial release sessions to address lingering muscle tightness that limits joint motion.
- Beyond two weeks: Incorporate strength training while continuing monthly deep‑tissue sessions for maintenance.
This combo reduces the risk of re‑injury and speeds up return to daily activities or sports.
When Massage Might Not Be Safe
Massage is powerful, but it isn’t a cure‑all. Avoid it (or get a therapist’s clearance) if you have:
- Active infection or open wounds near the joint.
- Severe osteoporosis; vigorous pressure could fracture bone.
- Blood‑clotting disorders or recent surgery without doctor approval.
- Acute inflammatory flare‑ups where heat and pressure worsen swelling.
In these cases, a qualified chiropractora practitioner focusing on spinal and joint alignment or a medical doctor should guide care first.
How to Choose the Right Massage Therapist
Not every practitioner is equipped to treat joint issues. Look for these credentials:
- Certification from a recognized body (e.g., AMTA, ABMP).
- Specialized training in sports or medical massage.
- Experience working with patients who have arthritis or orthopedic injuries.
- Willingness to communicate with your physical therapist or physician.
Ask for a brief consultation. A good therapist will assess your range of motion, ask about pain patterns, and propose a tailored plan.

Comparison of Massage Techniques for Joint Relief
| Technique | Primary Joint Benefit | Best For | Contraindications |
|---|---|---|---|
| Swedish | Improves circulation & reduces mild swelling | Early inflammation, general wellness | Severe heart conditions (heat) |
| Myofascial Release | Increases range of motion, releases adhesions | Chronic stiffness, post‑surgical scar tissue | Osteoporosis, acute fracture sites |
| Trigger Point | Alleviates referred joint pain from tight muscles | Muscle knots, overuse injuries | Open wounds, severe varicose veins |
| Deep‑Tissue | Breaks down dense scar tissue, strengthens connective tissue | Athletes, late‑stage rehab | Acute inflammation, blood‑clotting issues |
| Joint Mobilization | Directly improves joint capsule elasticity | Stiff knees, hips, shoulders | Recent joint replacement without clearance |
Quick Takeaways
- Massage boosts blood flow, reduces inflammation, and releases endorphins, all of which help joint repair.
- Choose the technique that matches your injury stage-light Swedish early, deeper myofascial later.
- Combine massage with physical therapy for the fastest, safest recovery.
- Always screen for contraindications like infection, severe osteoporosis, or recent surgery.
- Work with a certified therapist experienced in orthopedic or sports massage.
Frequently Asked Questions
Can massage replace medication for joint pain?
Massage can dramatically lower the need for painkillers, but it isn’t a wholesale replacement. Most doctors recommend using it alongside prescribed meds, especially during flare‑ups.
How often should I get a massage for arthritis?
A common schedule is once a week for the first six weeks, then taper to bi‑weekly as symptoms improve. Adjust based on how your joints feel.
Is deep‑tissue massage safe after a knee replacement?
Only after the surgeon clears you. Light myofascial work around surrounding muscles is usually fine, but direct pressure on the prosthetic joint should be avoided.
What should I tell my therapist before a session?
Mention any recent surgeries, current meds, and specific joint areas that hurt. Also note any conditions like blood clotting disorders or skin infections.
Can self‑massage help between professional visits?
Gentle self‑massage with a foam roller or massage ball can keep tissues supple and reduce stiffness, but it should never replace a therapist’s hands‑on assessment for deeper issues.

 Oct, 6 2025
Oct, 6 2025

Oliver Harvey
October 6, 2025 AT 15:34If you think a gentle rub can fix a busted joint, you might be in for a surprise. The reality is that technique matters more than the hype, and a proper myofascial release can actually shift the odds in your favor. Just don’t expect miracles after one session 😊
Ben Poulson
October 6, 2025 AT 23:54Dear readers, I wish to emphasize the significance of adhering to evidence‑based protocols when incorporating massage therapy into a joint rehabilitation regimen. It is imperative to select modalities that correspond with the physiological stage of tissue healing, thereby optimizing outcomes while mitigating adverse effects.
Raghav Narayan
October 7, 2025 AT 08:14Massage therapy offers a multifaceted approach to joint rehabilitation that extends beyond mere relaxation.
First, the mechanical stimulation of soft tissues enhances synovial fluid circulation, delivering nutrients directly to cartilage.
Second, the increased vascular perfusion supplies oxygen, which is essential for cellular repair processes.
Third, the rhythmic pressure applied during a session induces lymphatic drainage, thereby reducing interstitial edema that often hampers joint mobility.
Fourth, myofascial release specifically targets adhesions that tether muscles to the peri‑joint structures, restoring a more physiological range of motion.
Fifth, trigger point therapy alleviates myofascial hyperirritability, which frequently masquerades as joint pain.
Sixth, deep‑tissue techniques degrade fibrotic scar tissue that can form after surgery or repeated micro‑trauma.
Seventh, the neurochemical response includes the release of endorphins and serotonin, which modulate pain perception and improve mood.
Eighth, regular sessions create a conditioned relaxation response that can lower systemic inflammatory markers over time.
Ninth, when coordinated with a structured physical‑therapy regimen, massage accelerates the progression from passive to active strengthening phases.
Tenth, therapists who are certified in orthopedic massage can tailor the intensity and modality to the specific stage of healing, whether early inflammation or late remodeling.
Eleventh, the practitioner’s assessment of tissue quality often reveals asymmetries that may otherwise be missed in a standard clinical exam.
Twelfth, by addressing these asymmetries early, one can prevent compensatory movement patterns that predispose adjacent joints to injury.
Thirteenth, patient education during the session about proper joint mechanics reinforces the therapeutic gains achieved through manual work.
Fourteenth, documented outcomes in randomized trials indicate measurable improvements in pain scores and functional indices when massage is incorporated into a multimodal plan.
Finally, it is prudent to obtain medical clearance for individuals with contraindications such as active infection, severe osteoporosis, or uncontrolled coagulopathy, ensuring that the benefits outweigh any potential risks.
Tara Phillips
October 7, 2025 AT 16:34Esteemed colleagues, let us recognize that disciplined application of therapeutic massage not only ameliorates discomfort but also cultivates resilience within the musculoskeletal system; therefore, integrating scheduled sessions into one’s recovery plan is both prudent and empowering.
Derrick Blount
October 8, 2025 AT 00:54When examining, one must, without hesitation, consider, the profound, interrelation, between manual pressure, and the body's innate reparative mechanisms; consequently, the practitioner, should, meticulously, calibrate force, to align with the patient's current physiological state, thereby, maximizing therapeutic efficacy, while minimizing undue stress.
Anna Graf
October 8, 2025 AT 09:14Think of the body as a river; massage is the stone that smooths the banks, letting the water flow easier.
Jarrod Benson
October 8, 2025 AT 17:34Alright folks, picture this: you’re gearing up for a marathon, but your knees are screaming “stop!”-that’s where a solid massage plan swoops in like a superhero sidekick, loosening tight hamstrings, flushing out the lactic build‑up, and giving those joints the gentle push they need to keep moving forward, all while you stay pumped and ready to crush that finish line!
Liz .
October 9, 2025 AT 01:54Yo, if you’re looking to fix those achy knees just grab a therapist who knows the moves and keep it chill, no need for fancy talk.
tom tatomi
October 9, 2025 AT 10:14While many hail massage as a cure‑all, the data simply do not support such blanket claims; nonetheless, a measured approach may still offer adjunctive benefits when paired with conventional treatment.
Tom Haymes
October 9, 2025 AT 18:34Supporting a balanced regimen, incorporating massage after a strong warm‑up can enhance tissue pliability, and when combined with progressive loading, the joint's capacity to handle stress improves steadily.
Scott Kohler
October 10, 2025 AT 02:54Ah, the grand “force calibration” narrative-clearly the result of a shadowy syndicate of massage schools seeking to control our very perception of pain; one must remain vigilant and question the motives behind such pseudo‑scientific jargon.
Brittany McGuigan
October 10, 2025 AT 11:14Honestly, if we keep talking like a bunch of stiff n00bs, nobody'll actually take this stuff-real people need simple tips, not a lecture.
Priya Vadivel
October 10, 2025 AT 19:34Considering, however, the complex interplay of neurovascular responses, it is essential, to acknowledge, that massage can modulate, inflammatory cascades, thereby, offering a subtle yet measurable impact, even if skeptics prefer to dismiss it outright.
Dharmraj Kevat
October 11, 2025 AT 03:54Bro, think about it-muscles tight as rope, massage cuts the knot, joints breathe again.
Lindy Fujimoto
October 11, 2025 AT 12:14Honestly, I just told my therapist to “go wild” on my shoulders 😱🔥-the relief was unreal, and now I’m sharing the vibe, because everyone deserves that post‑massage glow! 🌟
darren coen
October 11, 2025 AT 20:34I appreciate the thorough overview.
Jennifer Boyd
October 12, 2025 AT 04:54Let’s all celebrate the power of a good massage-think of it as a warm hug for your joints, a boost of optimism that fuels your next workout, and a reminder that healing can be both gentle and heroic!
Lauren DiSabato
October 12, 2025 AT 13:14Everyone seems to think massage is just a feel‑good treat, but the truth is that without proper technique and timing, it’s basically wasted effort; so, if you’re serious about joint health, follow the protocols I’ve laid out, or you’ll just be spinning your wheels.