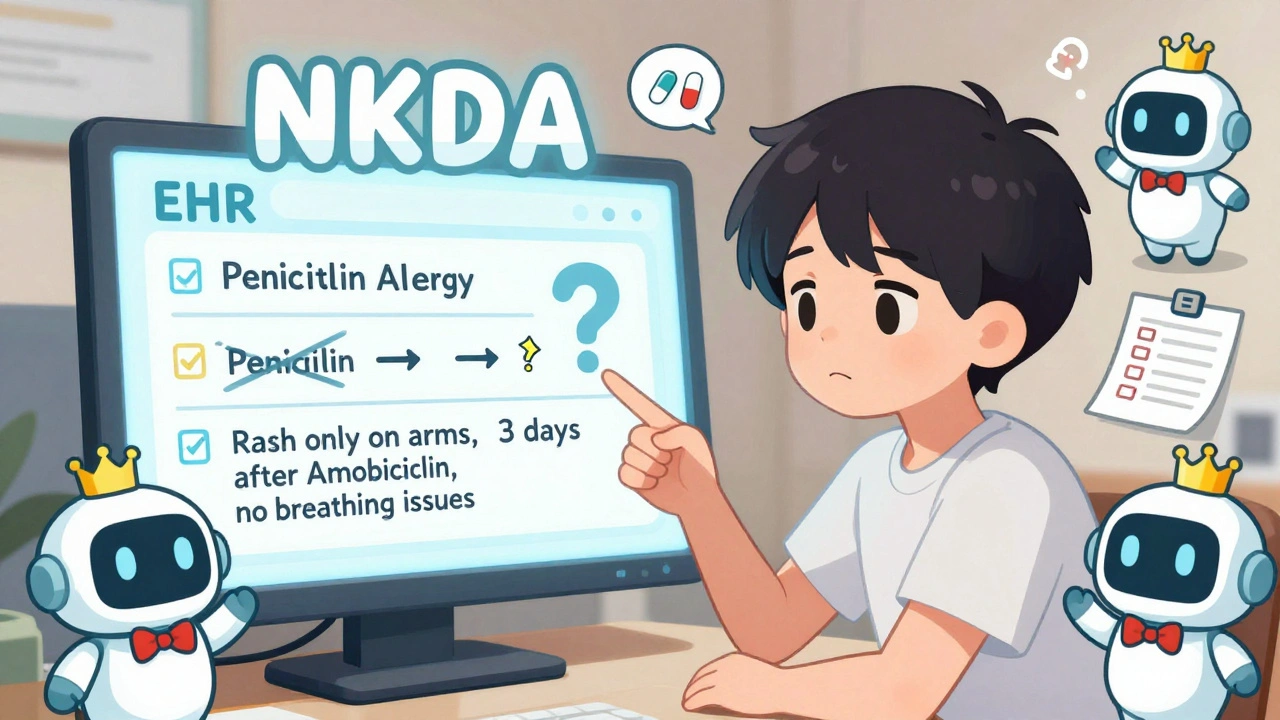
Every year, thousands of people in the U.S. end up in the emergency room because someone gave them a drug they’re allergic to - and it wasn’t because of a mistake by the doctor or nurse. It was because the allergy wasn’t written down clearly, or worse, wasn’t written down at all. If you’ve ever said, "I’m allergic to penicillin," but never explained what happened, you’re not alone. And you’re putting yourself at risk.
Why Your Allergy Info Needs to Be Specific
Saying "I’m allergic to sulfa" doesn’t tell your doctor enough. Maybe you got a rash after taking sulfamethoxazole for a urinary infection. Or maybe your throat swelled up after a shot of Bactrim. Those are two very different things. One might mean you can never take any sulfa drug again. The other might mean you just had a mild reaction - and you could safely take another one. The drug name matters. Use the generic name, not the brand. Say "ampicillin," not "Amoxil." Say "ibuprofen," not "Advil." Generic names are used in medical systems, and if your record says "penicillin" but the system only checks for "amoxicillin," you might get the wrong drug anyway. You also need to include:- What happened (rash, hives, trouble breathing, vomiting, anaphylaxis)
- How soon after taking the drug it started (within minutes? hours? days?)
- How severe it was (did you need epinephrine? hospitalization?)
What Your Medical Record Should Show - By Law
It’s not just a good idea. It’s required. The Centers for Medicare & Medicaid Services (CMS) says every patient’s chart must have a clear, up-to-date list of drug allergies. This applies to every hospital, clinic, and doctor’s office that takes Medicare or Medicaid. The rules say:- If you have allergies, they must be listed in a visible spot - usually the front of your chart or the top of your EHR screen.
- If you have NO known allergies, it must say "No Known Drug Allergies" (NKDA) - not just left blank.
- Every time you’re admitted or have surgery, your allergy list must be reviewed and confirmed - even if you’ve been there before.
Common Mistakes (And How to Fix Them)
Most people don’t know how to report allergies correctly. Here’s what happens a lot - and how to avoid it:- "I had a rash after penicillin." → That’s not enough. Was it itchy? Did it spread? Did you feel dizzy? Did it go away in a day? Write it all down.
- "I’m allergic to NSAIDs." → That’s too broad. Are you allergic to ibuprofen? Naproxen? Aspirin? Each one is different. Test one at a time if you’re unsure.
- "I was told I’m allergic to penicillin as a kid." → 90% of people who think they’re allergic to penicillin aren’t. A simple skin test can confirm it. If you never got tested, your record might be wrong - and you might be missing out on safer, cheaper antibiotics.
- "I don’t have any allergies." → Say it out loud. Even if you think you’re fine, tell your doctor. Then make sure they write "NKDA" in your chart.
What You Can Do Right Now
You don’t have to wait for your next appointment. Here’s how to fix your allergy record today:- Look at your last discharge summary, clinic note, or patient portal. Find the allergy section.
- Check if every drug is listed by its generic name.
- For each allergy, ask: Did I describe the reaction? Is it specific enough?
- If it’s vague - like "penicillin allergy" - write down exactly what happened. Use your phone notes if you need to.
- Call your doctor’s office. Ask them to update your record. Bring your written notes.
- If you’ve never been tested for penicillin allergy, ask about an allergy evaluation. It’s quick, safe, and often covered by insurance.
Why This Matters for You - Not Just the System
Your allergy record isn’t just paperwork. It’s your safety net. When you’re in the ER after a car crash, or being prepped for surgery, no one has time to ask you detailed questions. They look at your chart. If your allergy is listed as "penicillin," and they need to give you amoxicillin - which is in the same family - they might skip it. Even if you could have taken it safely. Or worse - they give you a drug you’re truly allergic to because your record says "no allergies" when it should say "anaphylaxis to ciprofloxacin." The Institute of Medicine estimated that better allergy documentation could prevent 7,000 deaths and 1.3 million injuries each year in the U.S. That’s not a guess. That’s based on real data from medication errors. Your record isn’t just for your doctor. It’s for every nurse, pharmacist, and ER doctor who touches your care. If you don’t make it clear, you’re the one who pays the price.
What’s Changing in 2025
By the end of 2023, all certified EHRs had to use a new standard called FHIR to share allergy data between systems. That means if you switch hospitals or doctors, your allergy info should follow you - if it’s entered right. In 2025, the Office of the National Coordinator for Health IT is rolling out new rules that will let you update your own allergy list through patient portals. You’ll be able to add reactions, upload notes from specialists, and even flag if an allergy has been ruled out. This is a big shift. You’re not just a patient anymore - you’re a co-manager of your safety. The tools are coming. But they only work if you use them.Final Tip: Don’t Trust Memory
People forget. Especially when they’re stressed. If you’ve ever had a reaction, write it down. Keep a copy on your phone. Print it. Give it to your primary care doctor. Make sure it’s in your chart. And if you’re ever unsure - ask. Say: "Can you check if my allergy is documented correctly?" Most doctors will be glad you asked. Your health isn’t complicated. But your records can be - if they’re sloppy. Clear, specific, and up-to-date allergy documentation isn’t just a rule. It’s the difference between a safe treatment and a life-threatening mistake.What should I write in my medical record if I think I’m allergic to a drug?
Write the exact generic drug name (like "sulfamethoxazole," not "sulfa"), the reaction you had (hives, swelling, trouble breathing), when it happened (minutes or hours after taking it), and how severe it was (did you need emergency care?). Avoid vague terms like "allergic to antibiotics" - be specific.
If I was told I’m allergic to penicillin as a child, do I still need to avoid it?
Not necessarily. About 90-95% of people who report a penicillin allergy aren’t truly allergic when tested. Many outgrow it, or had a side effect like nausea, not a real allergy. Ask your doctor about a penicillin allergy test - it’s simple, safe, and can open up better treatment options.
Does my allergy info automatically transfer when I change doctors?
Only if it’s entered correctly in a certified EHR system using the FHIR standard. Many systems still don’t share allergy data well. Don’t assume it transferred. Always confirm with your new provider and bring your own written list.
What if my doctor says I don’t need to document my allergy because it’s "not serious"?
Even mild reactions matter. A rash might seem harmless, but if you’re given the same drug again under stress (like during surgery), your body could react much worse. By law, every known reaction must be documented - no matter how minor it seemed at the time.
Can I update my allergy record myself?
Yes - and you should. Most patient portals let you view and request changes to your medical record. If you see a vague entry like "penicillin allergy," submit a message asking to clarify it with your reaction details. Keep a copy of what you sent. By 2025, new rules will make this even easier.

 Dec, 6 2025
Dec, 6 2025

Shayne Smith
December 6, 2025 AT 16:30Just updated my record after reading this. Wrote 'hives + dizziness 20 min after amoxicillin - ER visit' instead of 'allergic to penicillin'. Felt like a superhero.
Also printed it and stuck it on my fridge. My mom finally stopped asking if I'm 'still allergic to that one drug'.
Ibrahim Yakubu
December 7, 2025 AT 04:00You people are so naive. This isn't about documentation-it's about the pharmaceutical-industrial complex keeping you dependent. They want you scared of penicillin so you'll take their expensive alternatives. The '90% don't have real allergies' stat? That's a lab-funded lie. Real allergies don't disappear-they're suppressed by corporate medicine.
And FHIR? That's just another way for Epic to sell you more software while your data gets sold to insurers. Your 'safety net' is a trap. You think your chart is safe? It's being scraped, analyzed, and monetized while you're busy writing 'hives' in your portal.
And don't even get me started on the CDC's role in this. They're not protecting you-they're profiling you.
Billy Schimmel
December 8, 2025 AT 21:23My grandma had a rash after penicillin in 1972. They told her she was allergic. She never took it again. Died of sepsis at 84 because they gave her clindamycin instead. The doc didn't even check her chart.
So yeah. Write it down. Even if it's dumb. Even if it's old. Even if you think it's fine.
Just write it down.
Karen Mitchell
December 10, 2025 AT 00:00It is both morally and legally indefensible that patients are permitted to self-report drug allergies without objective diagnostic validation. The current system permits the proliferation of unsubstantiated, potentially dangerous, and clinically misleading data in electronic health records. This is not patient empowerment-it is medical anarchy.
There is no regulatory oversight of patient-submitted allergy claims. No verification. No accountability. And yet, we entrust life-or-death decisions to these unverified entries.
One must ask: if a patient claims an allergy to aspirin because they once got a stomachache after taking it, should a surgeon really be forced to avoid all NSAIDs? This is not safety-it is chaos masquerading as caution.
Until allergy documentation requires board-certified allergist confirmation, this entire framework is a farce.
Geraldine Trainer-Cooper
December 11, 2025 AT 02:05we're all just meat bags with wifi
your allergies are just your body screaming at the universe
but the system wants you to label it like a grocery list
penicillin = hives = bad
but what if it was just your soul rejecting capitalism
or maybe you were stressed and your immune system just needed a nap
they want you to write it down like it's a fact
but nothing is a fact
everything is a story
and your chart is just the first draft
update it if it makes you feel safe
but don't pretend you're controlling anything
you're just typing into the void
and the void is epic
and it's always listening
and it doesn't care if you got hives or not
Nava Jothy
December 12, 2025 AT 20:37OMG I just realized I’ve been living a lie 😭
I said "allergic to sulfa" for 12 years but never wrote down it was sulfamethoxazole and it was just a rash after a UTI… I’m basically a walking medical liability 😅
And I didn’t even know FHIR was a thing until now-how do people not know this?? I’m crying. I’m so embarrassed. I’ve been a bad patient. I need to call my doctor right now 💔
Also, if you’re not updating your allergies every 6 months, you’re not trying hard enough. This isn’t a hobby. This is survival. 💅
olive ashley
December 14, 2025 AT 19:43Let me guess-this whole post was paid for by Epic, right?
They need you to think your allergies are your problem so they don’t have to fix their broken EHRs.
Ever notice how every time you update your allergy, the system still doesn’t flag anything?
Or how your pharmacy still gives you amoxicillin even though you wrote 'anaphylaxis'?
This isn’t about you writing it down.
This is about hospitals refusing to train staff, labs refusing to share data, and insurance companies refusing to pay for allergy tests.
You’re being gaslit into blaming yourself while the real system fails.
And now you’re gonna go update your portal like a good little drone.
Good job. Keep doing what they told you to do.
Dan Cole
December 15, 2025 AT 00:41The entire premise of this article is dangerously oversimplified. Allergy documentation is not a matter of personal responsibility-it is a systemic failure of interoperability, clinical training, and regulatory enforcement.
It is statistically absurd to place the burden of accurate, granular, and temporally precise allergy reporting on laypersons who lack medical training, access to diagnostic tools, or even consistent healthcare.
Furthermore, the notion that '90% of penicillin allergies are false' ignores the fact that many patients have never been tested precisely because the healthcare system does not incentivize or fund such evaluations.
The FHIR standard is a technical improvement, but it does not address the root problem: providers are not trained to conduct structured allergy histories, and EHR vendors prioritize speed over safety.
And yet, we chastise patients for not being perfect data-entry clerks?
This is not empowerment. This is negligence dressed as education.
Fix the system, not the patient.