Lithium-NSAID Risk Calculator
How Risky Is This Combination For You?
This tool calculates your risk of lithium toxicity when taking NSAIDs based on key factors from medical research.
For millions of people taking lithium to manage bipolar disorder, a common pain reliever could be quietly damaging their kidneys-sometimes with life-threatening results. It’s not a rare scenario. Around 40 to 50% of long-term lithium users end up needing something for back pain, arthritis, or headaches. And for many, that something is an over-the-counter NSAID like ibuprofen or naproxen. What they don’t realize is that combining these two medications can spike lithium levels by up to 60%, leading to severe toxicity, acute kidney injury, or even permanent kidney damage. This isn’t a theoretical risk. It’s happening in real time, in clinics and ERs across the country, often because neither the patient nor the prescribing doctor fully understands how dangerous this combination is.
How Lithium and NSAIDs Interact
Lithium works by stabilizing mood, but it’s a narrow therapeutic drug. That means the difference between an effective dose and a toxic one is small. Your kidneys are responsible for clearing lithium from your body, and they do it slowly and carefully. NSAIDs-drugs like ibuprofen, naproxen, and indomethacin-shut down certain enzymes in the kidneys called cyclooxygenase (COX). These enzymes help produce prostaglandins, which keep blood flowing to the kidneys. When prostaglandins drop, kidney filtration slows down. And when kidney filtration slows, lithium doesn’t get flushed out. It builds up.
Studies show that within just 24 to 48 hours of starting an NSAID, lithium levels can jump by 20% to 60%. Indomethacin is the worst offender, often causing a 40% to 60% increase. Ibuprofen isn’t far behind, raising levels by 20% to 30%. Even celecoxib, often thought of as a "safer" NSAID, can still push lithium up by 10% to 15% in people with existing kidney issues. Aspirin and acetaminophen, on the other hand, have minimal effect. Acetaminophen is often the only safe alternative for pain relief in lithium users.
Why the Kidneys Take the Biggest Hit
The problem isn’t just about lithium levels rising. It’s about what happens when lithium and NSAIDs team up to attack the kidneys. Lithium alone can cause subtle damage over time-it interferes with how kidney cells handle sodium and water, leading to chronic changes. NSAIDs make this worse by reducing blood flow to the kidneys. Together, they create a double punch: one drug stresses the cells, the other starves them of oxygen and nutrients.
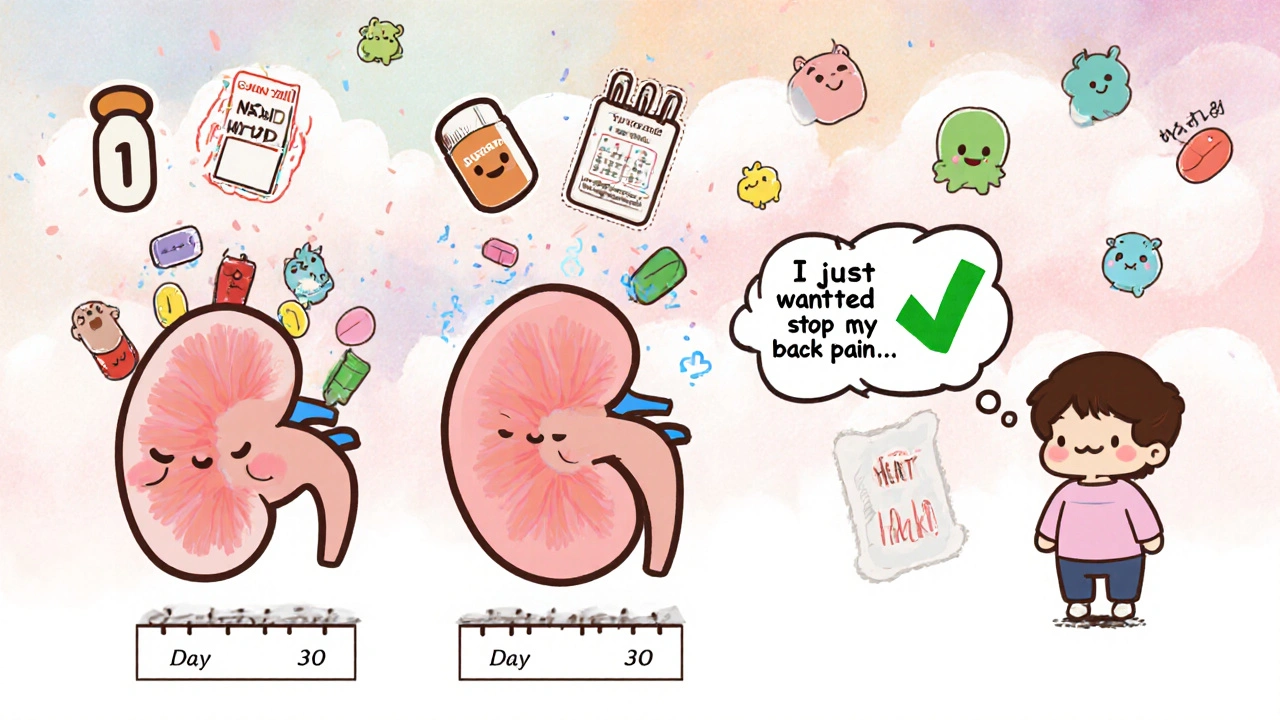
A 2023 study in JAMA Network Open found that people taking both lithium and an NSAID had more than a 3-fold higher risk of acute kidney injury compared to those on lithium alone. The highest risk? The first 30 days after starting the NSAID. That’s when lithium levels spike fastest and kidneys are most vulnerable. The damage isn’t always temporary. In one case series, 35% of patients who developed lithium-NSAID toxicity ended up with permanent kidney damage, defined as a 40% or greater drop in kidney function.
Who’s at the Highest Risk?
This isn’t a risk that affects everyone equally. Older adults are the most vulnerable. By age 65, kidney function naturally declines. Many lithium users are now over 50, and nearly 80% have other health conditions that require pain meds-osteoarthritis, back pain, migraines. A 2023 analysis of nephrology clinics found that over half of all lithium-related kidney injuries occurred in patients 65 and older.
People with preexisting kidney disease are in even greater danger. If your eGFR (a measure of kidney function) is already below 60 mL/min/1.73 m², even a small rise in lithium can push you into toxicity. And it’s not just age. Dehydration, heart failure, or taking diuretics can make the problem worse. Many patients don’t realize that even a few days of mild dehydration-like skipping water during a hot spell or having the flu-can trigger toxicity when combined with an NSAID.
What Symptoms Should You Watch For?
Lithium toxicity doesn’t always come with a warning. Early signs are easy to miss: slight hand tremors, mild nausea, or feeling more tired than usual. But these can quickly escalate. As lithium builds up, you might notice:
- Worsening tremors or muscle twitching
- Confusion, memory problems, or brain fog
- Slurred speech or difficulty walking
- Severe diarrhea or vomiting
- Seizures or loss of consciousness
These are emergency signs. If you’re on lithium and start taking an NSAID-even for a few days-and you notice any of these, get checked immediately. Lithium toxicity can progress from mild symptoms to coma or death in under 72 hours. Reddit forums and patient reports are full of stories where people took ibuprofen for a headache, felt off the next day, and ended up in the ER with lithium levels over 2.5 mEq/L (normal range is 0.6-1.2). One user described shaking so badly he couldn’t hold a cup of water. Another said he couldn’t remember his own address.
What Doctors Should Be Doing
Guidelines from the American Psychiatric Association, the American Society of Nephrology, and the European Psychiatric Association all agree: avoid NSAIDs in lithium users whenever possible. If you absolutely must use one, it should be for less than seven days, with close monitoring. That means checking lithium levels within 48 to 72 hours after starting the NSAID, and again after stopping it. Kidney function (creatinine and eGFR) should be checked weekly during that time.
And here’s the catch: many doctors don’t know this. A 2023 survey found that only 58% of primary care providers correctly identified NSAIDs as high-risk for lithium users. That’s why patients often get NSAIDs prescribed by their orthopedist, rheumatologist, or even their dentist-providers who aren’t thinking about psychiatric meds. Electronic health record alerts exist in most hospitals, but they only reduce co-prescribing by 35%. That means two out of three lithium users are still being handed NSAIDs without a warning.
What You Can Do Instead
If you’re on lithium and need pain relief, here’s what works:
- Acetaminophen (Tylenol) is the first choice. Stick to 3,000 mg per day max to avoid liver damage. It doesn’t affect lithium levels.
- Tramadol can be used cautiously if acetaminophen isn’t enough. Start low-25 mg daily-and increase slowly. It can raise lithium slightly, but not nearly as much as NSAIDs.
- Non-drug options like physical therapy, heat/cold packs, or acupuncture can help with chronic pain without any drug interaction.
- Short-term NSAIDs only-if absolutely necessary-and only with your psychiatrist’s approval. Use the lowest dose for the shortest time possible. Drink 3 liters of water a day while taking it.
And never assume an NSAID is safe just because it’s "over-the-counter." Just because you can buy it without a prescription doesn’t mean it’s harmless with lithium.
The Bigger Picture
This interaction isn’t just a medical footnote-it’s a systemic failure. The U.S. healthcare system spends nearly $50 million a year treating lithium-NSAID toxicity. Each hospitalization costs an average of $18,450. Yet, the problem persists because communication gaps between specialists are wide, patient education is weak, and many providers still treat NSAIDs as "harmless." Some health systems are making progress. Kaiser Permanente cut lithium-NSAID co-prescribing from 32% to under 12% by adding mandatory education and hard EHR alerts. The Veterans Health Administration, however, saw only a small drop, showing how inconsistent enforcement can be.
There’s also new research on the horizon. A 2023 clinical trial tested a new compound that protects kidney blood flow without interfering with lithium clearance. Early results were promising-87% fewer lithium spikes. But until that’s available, the safest path remains clear: avoid NSAIDs. Period.
Lithium is still the most effective medication we have for preventing suicide in bipolar disorder. It reduces suicide risk by 44%-far more than any alternative. That’s why millions will keep taking it. But if you’re one of them, your pain management plan needs to be just as carefully planned as your mood treatment. Don’t let a simple painkiller undo years of stability.
Can I take ibuprofen if I’m on lithium?
No, it’s not safe. Ibuprofen can raise lithium levels by 20% to 30%, increasing your risk of toxicity. Even a single dose can trigger symptoms like tremors, confusion, or nausea. If you need pain relief, use acetaminophen instead. If you’ve already taken ibuprofen, stop immediately and contact your doctor to check your lithium level.
How long does the lithium-NSAID interaction last?
The interaction doesn’t end when you stop the NSAID. It can take 7 to 10 days for kidney function to return to normal because prostaglandin levels stay suppressed. That means your lithium level may stay elevated for over a week after you stop taking the NSAID. Always monitor your lithium level during and after NSAID use.
Is celecoxib safer than other NSAIDs with lithium?
Celecoxib is less likely to raise lithium levels than ibuprofen or naproxen, but it still increases levels by 10% to 15%, especially in people with kidney problems. It’s not safe to assume it’s harmless. The safest approach is to avoid all NSAIDs, including celecoxib, unless under strict medical supervision.
What should I do if I accidentally took an NSAID while on lithium?
Stop taking the NSAID immediately. Drink plenty of water. Contact your psychiatrist or primary care provider right away to request a lithium blood test. If you’re experiencing tremors, confusion, vomiting, or dizziness, go to the ER. Don’t wait. Toxicity can develop quickly and become life-threatening within hours.
Are there any pain relievers that are completely safe with lithium?
Acetaminophen (Tylenol) is the only commonly used pain reliever that has no significant interaction with lithium. It’s the recommended first-line option. Opioids like tramadol can be used cautiously under supervision, but they’re not ideal for long-term use. Avoid all NSAIDs-including aspirin, naproxen, diclofenac, and meloxicam.
Why do some doctors still prescribe NSAIDs to lithium users?
Many doctors, especially outside of psychiatry, aren’t trained to recognize this interaction. A 2023 survey found that nearly 42% of primary care providers didn’t know NSAIDs were high-risk for lithium users. Patients often get NSAIDs from orthopedists, dentists, or ER doctors who don’t see their full medication list. Electronic alerts help, but they’re not foolproof. It’s up to you to speak up and ask: "Is this safe with lithium?"

 Nov, 12 2025
Nov, 12 2025

vanessa k
November 14, 2025 AT 01:26Lithium saved my life, but I didn’t know ibuprofen could kill my kidneys. I took it for a week last winter for a bad back and ended up in the ER with tremors so bad I dropped my coffee cup. No one warned me. Not my psychiatrist, not my orthopedist. Just a little blue pill and a headache. Now I keep Tylenol in every room. Never again.
manish kumar
November 14, 2025 AT 18:06As someone who’s been on lithium for 14 years and also deals with chronic knee pain from years of manual labor, I’ve had to relearn everything about pain management. I used to pop naproxen like candy-until I read a study that said NSAIDs reduce glomerular filtration rate by up to 30% in long-term lithium users. That’s not just a side effect, that’s a slow-motion kidney collapse. Now I do physical therapy twice a week, use heat wraps, and swear by acetaminophen. It’s not glamorous, but it’s the only way I’ve stayed off dialysis. If you’re on lithium, treat your kidneys like they’re made of glass-because they are.
Nicole M
November 15, 2025 AT 18:35Wait, so celecoxib isn’t safe either? I thought it was the ‘gentle’ NSAID. I’ve been taking it for my arthritis for two years. Am I already damaged?
Arpita Shukla
November 15, 2025 AT 20:50Actually, you’re probably fine if your eGFR is above 60. But if you’re over 60, dehydrated, or on diuretics, even celecoxib can push you into toxicity. The JAMA study showed 35% of patients with preexisting kidney issues developed permanent damage after just one NSAID course. You should’ve gotten a baseline creatinine test before starting it. And yes, you need to get it checked now. Don’t wait for symptoms.
Benjamin Stöffler
November 17, 2025 AT 20:47It’s not the NSAIDs. It’s not even the lithium. It’s the system. The system that allows over-the-counter drugs to be sold without context. The system that trains orthopedists to treat pain, not pharmacology. The system that assumes patients are literate in drug interactions. We’ve turned healthcare into a vending machine: insert symptom, receive pill. No counseling. No warnings. No accountability. And now, people are dying because we outsourced responsibility to a pill bottle. Wake up.
Mark Rutkowski
November 19, 2025 AT 00:31Lithium isn’t just a mood stabilizer-it’s a lifeline for people who’ve stared into the abyss and come back. And yet, we treat it like an afterthought. Meanwhile, a $2 bottle of ibuprofen gets more shelf space than a decade of psychiatric research. We’ve got a drug that cuts suicide risk by 44%, and we’re letting people accidentally poison themselves with painkillers bought next to chewing gum. This isn’t negligence-it’s moral laziness. We owe it to the people who survive bipolar disorder to protect them from the very things meant to help them feel better.
Ryan Everhart
November 20, 2025 AT 14:32So… Tylenol is the answer? Cool. I guess we just need to trade one potential liver failure for a guaranteed kidney failure. Thanks, medicine.
David Barry
November 21, 2025 AT 08:43Acetaminophen isn’t safe either if you drink. Or if you’re obese. Or if you’re on any other hepatic enzyme inducers. You’re just swapping one risk for another. The real answer? No pain meds. Just endure. Or die. Pick one.