Seasonal Allergy Symptom Checker
Select Your Symptoms:
Your Allergy Analysis
Enter your pollen count and select symptoms to get personalized recommendations.
When seasonal allergies are a recurring set of symptoms triggered by airborne pollen, mold spores, or other environmental irritants that flare up at certain times of the year, life can feel like a constant sneeze‑fest. The good news? You don’t have to suffer in silence. By combining smart medication choices, indoor‑environment tweaks, and a few natural tricks, you can keep the sniffles, itchy eyes, and congestion under control.
Quick Takeaways
- Track local pollen counts and plan outdoor activities for low‑pollen windows.
- Choose non‑drowsy antihistamines for daytime relief; add a nasal corticosteroid spray for persistent stuffiness.
- Invest in a HEPA‑rated air purifier and keep windows closed on high‑pollen days.
- Wash clothing and shower after being outside to rinse off pollen.
- Consider immunotherapy if OTC options aren’t enough.
What Triggers Seasonal Allergies?
Understanding the root cause helps you attack the problem directly. The main culprit is pollen count the measured concentration of pollen grains in the air, reported hourly by weather services and allergy apps. When counts rise, your immune system mistakenly flags pollen as a threat, releasing histamine a chemical that widens blood vessels and triggers itching, swelling, and mucus production. The result: itchy eyes, runny nose, and that classic post‑nasal drip.
Other seasonal triggers include mold spores that thrive in damp weather, and even certain weeds that release pollen later in the year. Knowing which plants dominate your region (tree pollen in spring, grass in early summer, ragweed in late summer) lets you anticipate symptom spikes.
Medication Options That Actually Work
Over‑the‑counter (OTC) meds are the first line of defense, but choosing the right type matters.
Antihistamines
Antihistamines are drugs that block the histamine receptors, preventing the cascade that leads to allergy symptoms. Non‑drowsy formulations like loratadine or fexofenadine are ideal for daytime use. If you need a stronger kick, cetirizine works well but may cause mild sleepiness for some.
Nasal Corticosteroid Sprays
Nasal corticosteroid sprays reduce inflammation inside the nasal passages, addressing congestion and runny nose at the source. Brands such as fluticasone or budesonide are safe for daily use. Start a few weeks before the season kicks in for maximum benefit.
Decongestant Pills and Sprays
Short‑term use of pseudoephedrine pills or oxymetazoline nasal sprays can unclog a stuffy nose, but keep them under 3‑4 days to avoid rebound congestion.
Comparison: OTC vs Prescription Antihistamines
| Attribute | OTC Options | Prescription Options |
|---|---|---|
| Typical Uses | General seasonal symptoms | Severe or chronic allergy cases |
| Onset Time | 30‑60 minutes | 15‑30 minutes |
| Drowsiness Risk | Low (non‑drowsy) to moderate | Varies - some are more sedating |
| Price (USD) | $10‑$25 per month | $30‑$70 per month |
Home & Lifestyle Strategies
Medication helps, but controlling your environment reduces the load on your immune system.
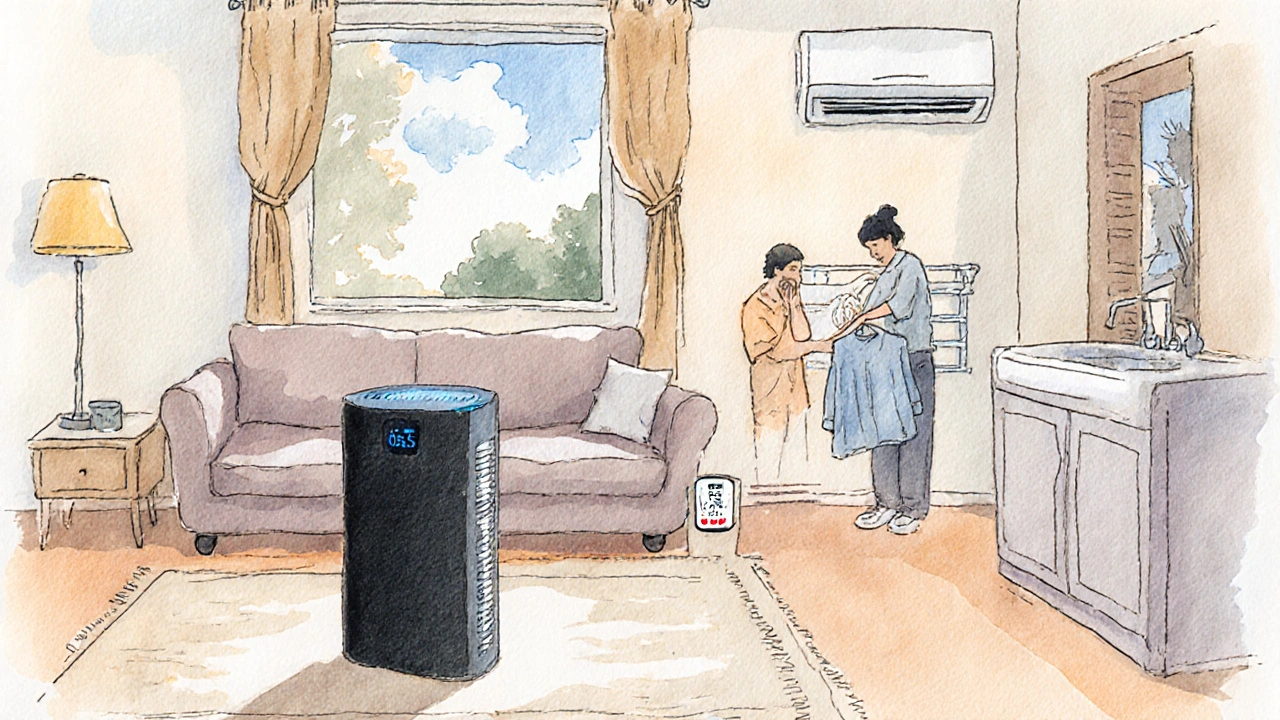
Air Purifiers and HEPA Filters
Air purifiers devices equipped with HEPA (High Efficiency Particulate Air) filters that capture particles as small as 0.3 microns, including pollen and mold spores are worth the investment. Place one in the bedroom and living area, run it on high during high‑pollen days, and change the filter every 6‑12 months.
Keep Windows Closed & Use AC
When outdoor pollen counts exceed 50 grains per cubic meter, keep windows shut and run the air conditioner on the recirculate setting. The AC’s built‑in filter catches many allergens before they enter the home.
Shower & Change Clothes After Outdoor Activities
Pollen sticks to hair and clothing. A quick shower and a fresh shirt can prevent that pollen from migrating to your bedroom pillows and mattress.
Humidity Control
Maintain indoor humidity between 30‑50%. Too dry aggravates nasal passages, while too humid encourages mold growth. A small hygrometer and a dehumidifier (if needed) keep the balance.
Natural Remedies & Supplements
Some people find relief with botanical or nutritional aids, though they should complement-not replace-meds.
- Quercetin: a flavonoid found in apples and onions that stabilizes mast cells, potentially lowering histamine release. Typical dose: 500mg twice daily.
- Probiotic strains such as Lactobacillus rhamnosus have shown modest benefit in reducing allergic inflammation in several clinical trials.
- Butterbur extract (Petasites hybridus) can match antihistamines for nasal symptoms, but avoid raw butterbur due to liver‑toxicity concerns.
Always check with a healthcare provider before starting supplements, especially if you’re on prescription meds.
When to Consider Immunotherapy
If OTC options and lifestyle tweaks leave you still sniffling, immunotherapy is a long‑term treatment that gradually desensitizes the immune system to specific allergens through regular injections or sublingual drops may be the answer. It usually requires a 3‑5 year commitment but can cut medication needs dramatically.
Eligibility criteria include:
- Confirmed allergy via skin‑prick or specific IgE testing.
- Symptoms persisting despite optimal OTC and environmental control.
- Willingness to attend regular appointments.
Talk to an allergist to see if a tailored immunotherapy plan fits your situation.
Seasonal Allergy Checklist
- One week before the season: Start a non‑drowsy antihistamine and a nasal corticosteroid spray.
- Morning: Check the local pollen count on a weather app. If > 50, keep windows closed.
- Before stepping out: Wear sunglasses and a light mask if you’re highly sensitive.
- After returning home: Shower, change clothes, and wipe down hair with a damp towel.
- Evening: Run the air purifier on high for 30minutes, then clean the filter weekly.
- Weekly: Wash bedding in hot water (130°F) to kill trapped pollen.
- Monthly: Review symptom diary. If meds aren’t enough, schedule an allergist visit.

Frequently Asked Questions
Can I take antihistamines every day?
Yes, most non‑drowsy antihistamines are safe for daily, year‑round use. If you notice side effects, switch to a different brand or discuss a prescription option with your doctor.
Do natural supplements replace medication?
They can lessen symptoms for some people but usually work best alongside proven meds. Use supplements as an adjunct, not a substitute.
How often should I change my air purifier filter?
Most manufacturers recommend replacing HEPA filters every 6‑12 months, or sooner if the indicator light turns on during heavy pollen periods.
Is immunotherapy painful?
Allergy shots involve a quick injection under the skin; most people feel only a mild pinch. Sublingual tablets dissolve under the tongue and are completely pain‑free. Both methods can cause temporary swelling at the site.
What’s the best time of day to take antihistamines?
Take them with a glass of water after breakfast. This timing maximizes absorption and reduces the chance of stomach upset.

 Oct, 1 2025
Oct, 1 2025
Christine Watson
October 1, 2025 AT 23:10Great rundown! I’ve found that checking the pollen count first thing in the morning really helps me schedule my jogs. Using a HEPA filter in the bedroom cuts down nighttime sniffles, and I never skip the nightly shower after a hike. Pairing a non‑drowsy antihistamine with a nasal spray before the season hits has kept my eyes clear all spring.
Macy Weaver
October 3, 2025 AT 16:00I love how the article blends practical steps with a bit of science. Adding a probiotic like Lactobacillus rhamnosus can subtly modulate the immune response, which many people overlook. Keeping indoor humidity between 30‑50% not only curbs mold but also prevents the nasal passages from drying out. When you wash your bedding in hot water weekly, you’re essentially flushing out the pollen that settled overnight. Remember, consistency is key; the body rewards steady habits more than occasional heroics.
James McCracken
October 4, 2025 AT 19:46While the guide praises antihistamines, one could argue that muddling your immune response with chemicals is a misguided shortcut.
Evelyn XCII
October 5, 2025 AT 23:33Oh great, another list of 'must‑do' steps-because we all have time to wash bedding after every sneeze. Not like we’re living in a dust‑free utopia.
Suzanne Podany
October 7, 2025 AT 03:20Think of allergy management as a team sport, where every habit you adopt passes the ball to the next defense line. Start by checking the local pollen index on a reliable app-this data is free and accurate. Pair that knowledge with a HEPA filter in the bedroom and you’ve already set up a solid goalpost. Don’t forget to rinse off pollen from hair and clothes before you hit the sheets; it’s a small step with big payoff. Over time, these collective actions create a healthier environment for everyone in your household.
Nina Vera
October 8, 2025 AT 07:06When the pollen count spikes, I feel like the universe is conspiring against my morning coffee. I scramble to close every window, even the tiny ones in the bathroom, as if the walls themselves might exhale allergens. The air purifier hums like a loyal guardian, yet it seems to sigh every time a new sneeze erupts. I slap on my sunglasses and a light mask, turning myself into a reluctant superhero battling invisible pollen villains. The first wave of sneezing hits, a relentless drumbeat that rattles my teeth and makes my throat feel like sandpaper. I reach for the non‑drowsy antihistamine, pop it like a tiny shield, and hope it will stall the assault. Meanwhile, my nose produces a river of mucus that seems to defy gravity, dripping onto my shirt and staining my confidence. I sprint to the bathroom, wash my hair, and scrub my hairline, as if shampoo could wash away the pollen that clings like glitter. By the time I’m dressed again, I’m already counting the minutes until the next high‑pollen forecast. The evening arrives, and I finally let the air purifier run on turbo, listening to its whir as a lullaby for my inflamed sinuses. I change the filter, a ritual that feels like swapping out the armor of a knight before the next battle. I lay down, pull the blankets over my face, and try to persuade my brain that the world outside is just a distant rumor. Sleep creeps in, but every twitch feels like another pollen particle trying to sneak past the fortress. When I wake, the cycle begins anew, a relentless loop that tests my resolve day after day. Yet, amidst the chaos, I find a strange satisfaction in mastering this seasonal siege, knowing each small victory-like a clear eye or an unblocked nostril-is a triumph over nature’s whims.
Christopher Stanford
October 9, 2025 AT 10:53Let’s be honest: the supplement section reads like a marketing brochure written by a salesman on a sugar high. Quercetin’s bioavailability is notoriously low, and most over‑the‑counter brands skimp on the dose needed for any real effect. Butterbur, while promising, carries a hidden risk of hepatotoxicity if the extract isn’t fully processed. The article fails to flag these caveats, leaving vulnerable readers to gamble with their liver. A critical eye would demand links to peer‑reviewed studies, not just anecdotal claims. Bottom line: stick to proven meds first, and treat supplements as optional add‑ons under physician guidance.
Steve Ellis
October 10, 2025 AT 14:40Hey team, you’ve got this! Treat your daily antihistamine like a warm‑up before a big game-consistent and purposeful. If congestion is dragging you down, think of a nasal spray as a tactical timeout that clears the field. Keeping your living space clean is the equivalent of maintaining a tidy locker room; it just makes performance smoother. Celebrate each small win, whether it’s a sneeze‑free meeting or a clear‑sighted hike.
Jennifer Brenko
October 11, 2025 AT 18:26From a patriotic standpoint, protecting our citizens from invasive pollen is a matter of national health security. The government's investment in public pollen monitoring stations should be expanded to safeguard every community. Failure to act decisively undermines our collective wellbeing.
Harold Godínez
October 12, 2025 AT 22:13Just a heads‑up: the article switches between 'allergy' and 'allergies' a lot-pick one and stick with it. Also, 'air purifier' should be plural when you’re talking about multiple devices. The bullet list could use consistent punctuation; some items end with periods, others don’t. Minor tweaks, but they make the guide look sharper.
Sunil Kamle
October 14, 2025 AT 02:00It is with great enthusiasm that we observe yet another exhaustive list of preventative measures, as if humanity had not previously discovered the virtues of staying indoors. One must, of course, applaud the ingenuity of recommending sunglasses for pollen protection-a truly avant‑garde solution. Nonetheless, the prose retains a charmingly pedantic tone that is, regrettably, wholly necessary.
Michael Weber
October 15, 2025 AT 05:46The human condition, perpetually besieged by microscopic wanderers, mirrors our existential struggle against unseen forces. Each sneeze is a reminder of our fragility, a fleeting gasp in the theater of life. By medicating, we merely postpone the inevitable confrontation with nature's indiscriminate design. Yet, there is a certain catharsis in the ritual of showering off pollen, as if cleansing the body might also purge the soul. Ultimately, true mastery lies not in suppression but in harmonious coexistence with the airborne world.
Blake Marshall
October 16, 2025 AT 09:33U dont need 10 different meds, just one good antihistine does the trick. Also, dnt forget to close the windows!
Shana Shapiro '19
October 17, 2025 AT 13:20I understand how relentless the seasonal onslaught can feel, like a storm that refuses to give you respite. Your dedication to following each recommendation is commendable, even when the symptoms seem insurmountable. The nightly ritual of showering and changing clothes is a powerful act of self‑care, a quiet rebellion against the pollen’s tyranny. Remember that the air purifier’s gentle hum is not merely a machine, but a steadfast ally in your fight. Should you ever feel overwhelmed, pause and breathe deeply; the body often steadies itself when given a moment of calm. Your perseverance will undoubtedly turn these challenges into triumphs.
Jillian Bell
October 18, 2025 AT 17:06Behind the polished advice lies a hidden agenda pushing pharmaceutical profits while keeping us dependent on endless prescriptions. The pollen data shared publicly is filtered, omitting spikes that would expose governmental negligence. Natural immunity is systematically suppressed through mandatory antihistamine campaigns. Stay vigilant, question the source, and protect your autonomy.
Lindsey Bollig
October 19, 2025 AT 20:53Great points, Jennifer-especially the call for stronger public health measures. Implementing more localized pollen monitoring could indeed make a big difference.