Statin drugs have saved millions of lives by lowering cholesterol and preventing heart attacks. But for a significant number of people, the benefit comes with a painful trade-off: muscle pain. This isn't just ordinary soreness. It can be persistent, debilitating, and sometimes mistaken for something else entirely. If you're on a statin and suddenly feel like your muscles are constantly achy, weak, or cramping - especially if it started after you began the medication - you're not imagining it. You might be experiencing statin-induced myopathy, a spectrum of muscle problems that range from mild discomfort to a rare but serious autoimmune condition.
What Exactly Is Statin-Induced Muscle Pain?
Statin-induced muscle pain falls under a broad category called statin myopathy. It's not one single problem - it's a range of reactions, from simple discomfort to severe muscle damage. The most common form is myalgia, which means muscle pain without any measurable muscle damage. You feel sore, stiff, or weak, but your blood tests - especially creatine kinase (CK) - stay normal. This affects up to 30% of people taking statins, according to the American College of Cardiology. Many assume it's just aging or overexertion. But if the pain appeared after starting the statin and goes away after stopping it, the link is likely real.
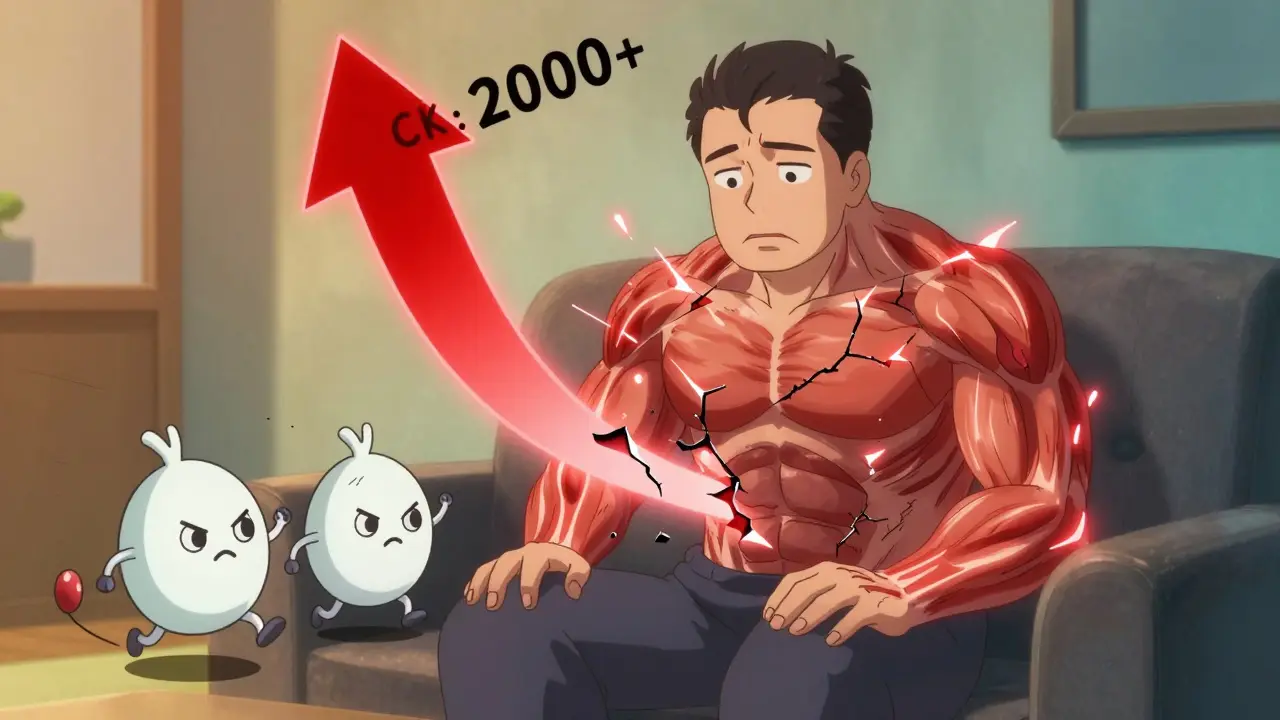
Then there's myositis, a more serious version. This isn't just pain - it's inflammation. Your CK levels rise, often 10 to 40 times above normal. Your muscles are breaking down. You might notice trouble climbing stairs, lifting your arms, or even standing up from a chair. Unlike myalgia, this isn't something you can just "sleep off." It requires medical attention.
At the extreme end is rhabdomyolysis, a medical emergency. This happens when muscle tissue breaks down so badly that it releases proteins into your bloodstream, which can overload your kidneys. CK levels spike over 40 times the upper limit of normal. You might see dark, tea-colored urine. This is rare - affecting only 0.01% to 0.1% of statin users - but it can lead to kidney failure if not treated fast.
The Hidden Culprit: How Statins Damage Muscle
Statins work by blocking an enzyme called HMG-CoA reductase. This cuts cholesterol production in the liver. But here's the catch: that same enzyme is involved in making other vital compounds - not just cholesterol. One of them is coenzyme Q10 (CoQ10), which your muscles need to produce energy. Studies show that taking 40 mg of simvastatin daily can reduce CoQ10 levels in muscle tissue by as much as 40%. That means your muscle cells are running on low battery.
Statins also interfere with something called protein prenylation. This process helps regulate calcium inside muscle cells. When it's disrupted, calcium levels rise abnormally - from the normal 100 nM to 150-200 nM. High calcium triggers enzymes that chew up muscle proteins. Add in exercise, especially eccentric movements like downhill walking or lowering weights, and the damage accelerates. Muscle biopsies show that statins crank up the body's natural waste disposal system - the ubiquitin-proteasome pathway - by 300-400%. Your muscles aren't just tired; they're being actively broken down.
The Rare but Dangerous Form: Immune-Mediated Necrotizing Myopathy
There's another layer to statin muscle pain that most people - even many doctors - don't know about. It's called immune-mediated necrotizing myopathy (IMNM), or statin-associated autoimmune myopathy (SAAM). This isn't a side effect - it's an autoimmune disease triggered by the drug.
Here's how it happens: In some people, statins cause muscle cells to overproduce the very enzyme the drug is meant to block - HMG-CoA reductase. The immune system sees this as a foreign invader and starts attacking it. Antibodies form against HMG-CoA reductase (anti-HMGCR antibodies). These antibodies then go after your own muscle tissue, causing progressive weakness that gets worse over time.
Unlike regular statin myopathy, this doesn't go away when you stop the drug. In fact, symptoms often get worse. About half of patients continue to struggle for 6 to 12 months after quitting statins. Muscle biopsies show dead muscle fibers with almost no inflammation - a telltale sign. CK levels are sky-high, often over 2,000 IU/L (normal is 30-200). This form mostly hits people over 50. Genetics play a role too - 70% of cases have a specific gene variant called HLA-DRB1*11:01.
Diagnosis: It’s Not Just a Blood Test
Many patients are misdiagnosed for months - even years. On forums like Myositis Support and Understanding, 68% of SAAM patients say they were first told they had fibromyalgia or chronic fatigue syndrome. The average delay in diagnosis? Over 11 months.
Here's what real diagnosis looks like:
- Stop the statin. If symptoms improve within 1-2 weeks, it's likely myalgia. If they persist or worsen, dig deeper.
- Check CK levels. Normal? Probably myalgia. Elevated? Could be myositis. Very high? Watch out for rhabdomyolysis or SAAM.
- Test for anti-HMGCR antibodies. This is the key test for autoimmune myopathy. If positive, you're dealing with SAAM.
- Get a muscle biopsy. The gold standard. It shows necrotic fibers with little inflammation - the fingerprint of SAAM.
- Check other causes. Thyroid issues, low vitamin D, and drug interactions (like with amiodarone) can mimic statin myopathy.
Electromyography (EMG) and muscle MRI also help. EMG shows myopathic changes in 80% of confirmed cases. MRI reveals swelling in the hip and shoulder muscles - areas most commonly affected.
Treatment: One Size Doesn’t Fit All
What you do next depends entirely on what you’re dealing with.
For myalgia: Many people can switch to a different statin. Rosuvastatin (Crestor) or pravastatin (Pravachol) are often better tolerated. Dosing changes help too - going from daily to every-other-day dosing works for 40% of patients. Some find relief with CoQ10 supplements (200 mg/day), though studies show mixed results.
For myositis: Stop the statin. Give your body time to heal. Most recover fully in a few weeks. Avoid intense exercise until CK levels normalize.
For SAAM (immune-mediated): This is not a simple case of stopping a drug. You need immunosuppression. Standard treatment is high-dose prednisone (1 mg per kg of body weight daily) plus either methotrexate or mycophenolate. About 60-70% of patients go into remission within a year. If that fails, IVIG (intravenous immunoglobulin) or newer drugs like ravulizumab (a complement inhibitor) are showing promise. Delaying treatment? Big mistake. Patients treated within 6 months of symptoms have a 65% chance of full recovery. If you wait over a year, that drops to 28%.
Who’s at Higher Risk?
Not everyone is equally likely to develop statin muscle problems. Risk factors include:
- Age over 65
- Female sex
- Small body frame
- Chronic kidney disease
- Drug interactions - especially with amiodarone, fibrates, or certain antibiotics
- Genetic variants like SLCO1B1 rs4149056 - this increases simvastatin myopathy risk from 0.6% to 1.4%
- African American descent - studies show 1.8 times higher risk than Caucasians
Interestingly, atorvastatin (Lipitor) shows up in over 43% of statin myopathy reports to the FDA - even though it's prescribed less than half as often as simvastatin. Why? Probably because it's the most widely used statin overall. But the risk is real.
What Happens If You Just Quit?
Stopping statins might fix the muscle pain - but it leaves your heart vulnerable. A 2023 study in Circulation found that people who quit statins due to muscle pain had a 25% higher risk of heart attack or stroke over the next 10 years. That’s huge. You can’t just walk away from cardiovascular protection.
The goal isn’t to avoid statins entirely. It’s to find a version and dose that works for you. For many, switching statins, lowering the dose, or changing the schedule makes all the difference. For others with SAAM, the solution is stronger - immunosuppressants - not avoidance.
The Future: Personalized Statin Therapy
Scientists are moving toward smarter prescribing. A 2024 American Heart Association statement predicts that within five years, we’ll use genetic testing to match patients with the statin safest for their body. Polygenic risk scores could cut myopathy rates by 30-40%. Blood tests for microRNAs (like miR-206 and miR-133a) are already being validated to tell apart autoimmune myopathy from regular muscle pain - with 89% accuracy.
The message is clear: muscle pain on statins isn’t something to ignore. It’s not "just a side effect." It’s a signal. And how you respond to it - whether you stop, switch, or seek specialist care - can make the difference between a healthy heart and a broken muscle.

 Feb, 21 2026
Feb, 21 2026
