Head Injury Urinary Retention: Causes, Assessment, and Management
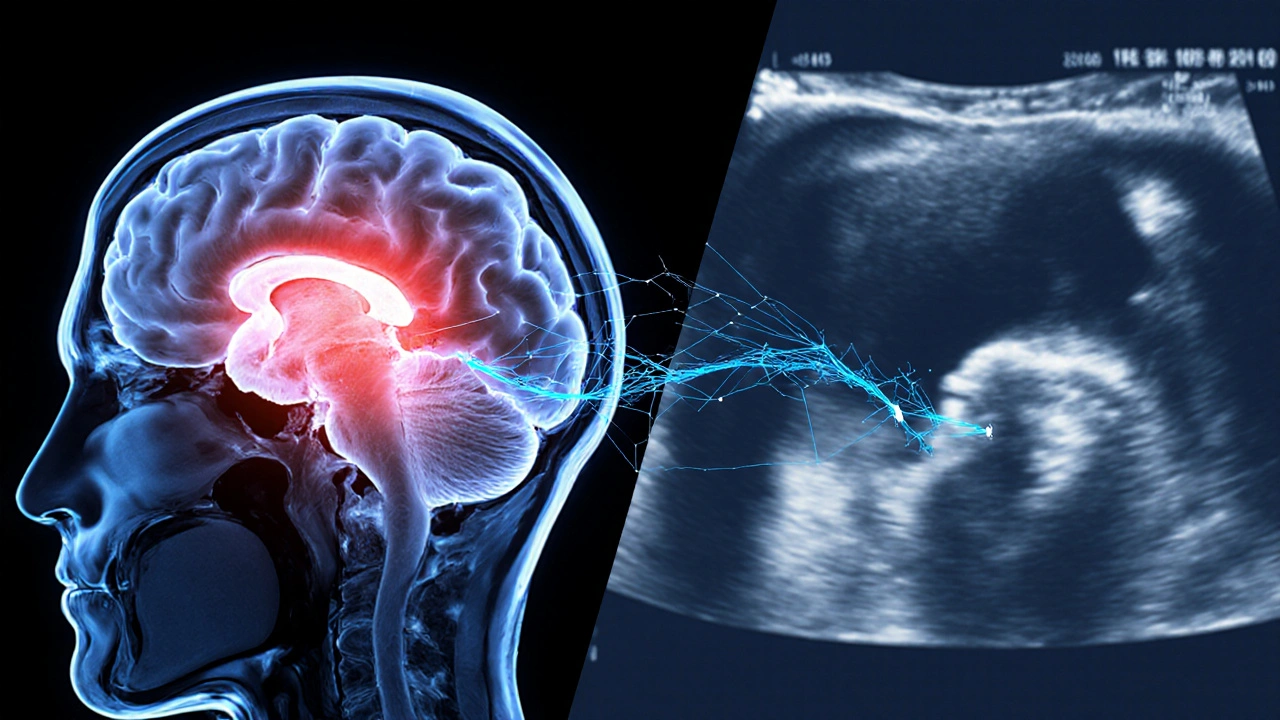
When dealing with head injury urinary retention, the inability to empty the bladder that follows a traumatic brain event. Also known as neurogenic urinary retention after head trauma, it bridges two distinct medical areas: the direct effects of head injury, and the downstream problem of urinary retention. The condition typically arises because the brain injury disrupts the nervous pathways that tell the bladder when to contract, a situation clinicians label as neurogenic bladder. In plain terms, the brain‑to‑bladder communication line gets scrambled, so the bladder either never gets the signal to empty or the signal is too weak. This link is the core of the semantic triple: head injury can cause urinary retention. Understanding this cause‑effect chain helps you spot early warning signs—hesitancy, weak stream, or a full‑feeling bladder that won’t go away. Once you recognize the pattern, you can move quickly to the next triple: urinary retention often results from neurogenic bladder dysfunction, which means a focused neurological exam and bladder scan become essential tools. Treatment doesn’t start with medication alone; it begins with a clear assessment plan that includes imaging of the brain, neurologic reflex testing, and measurement of post‑void residual volume. From there, a multidisciplinary approach—often involving a urologist, neuro‑rehabilitation therapist, and a pharmacist—addresses both the root brain injury and the bladder’s response. The goal is to restore safe emptying, prevent kidney damage, and improve quality of life, all while keeping medication side‑effects in check.
Key Factors and Practical Steps
First, identify the severity of the head injury using established scales like the Glasgow Coma Scale; severe injuries carry a higher risk of bladder control loss. Second, evaluate the urinary retention with a simple bedside bladder scanner—most clinics can spot a residual volume over 150 ml, which signals a problem. Third, consider the role of neurogenic bladder types: are you dealing with an underactive bladder, an overflow pattern, or a combination? This classification guides the next semantic triple: managing head injury urinary retention requires medication review. Common culprits include anticholinergics, opioids, and certain antihypertensives that can further blunt bladder contractions. Adjusting doses, switching to bladder‑friendly alternatives, or adding a cholinergic agent can make a noticeable difference. Non‑pharmacologic options—scheduled voiding, timed catheterization, and pelvic floor training—often work hand‑in‑hand with drug therapy. In more stubborn cases, intermittent catheterization or a permanent catheter may be necessary, but only after weighing infection risk and patient comfort. Throughout, keep an eye on kidney function tests; chronic retention can lead to hydronephrosis, a silent threat that shows up as rising creatinine. Finally, document progress with regular post‑void residual checks and symptom logs; this data fuels the ongoing decision‑making loop and helps your care team fine‑tune the plan.
All of these pieces—injury grading, bladder assessment, medication tweaks, and supportive therapies—come together to form a comprehensive roadmap for anyone facing head injury urinary retention. Below, you’ll find a curated list of articles that dive deeper into medication safety, neurological symptom monitoring, and practical treatment tips. Whether you’re a patient trying to understand why you can’t empty your bladder, a caregiver looking for actionable steps, or a clinician seeking a quick reference, the posts ahead cover the most relevant drugs, diagnostic tools, and lifestyle adjustments you’ll need to manage this complex condition effectively.

 Sep, 30 2025
Sep, 30 2025