Traumatic Brain Injury Bladder: What You Need to Know
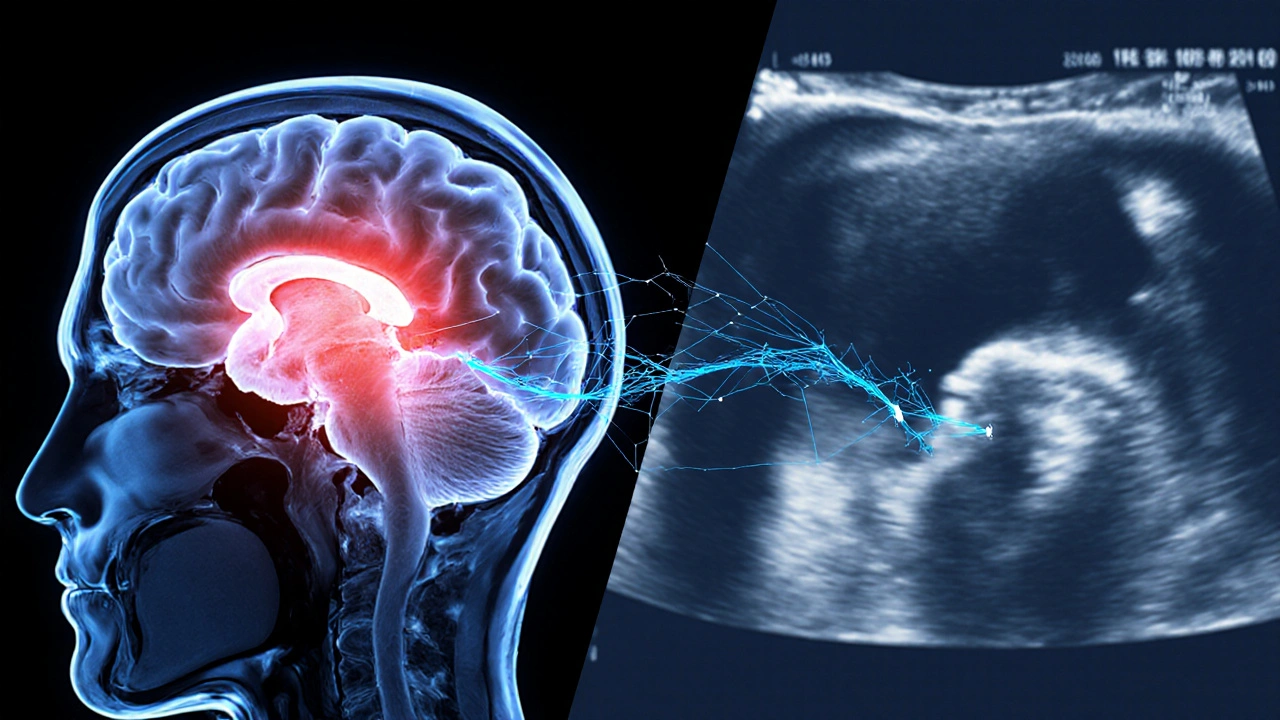
When dealing with Traumatic Brain Injury Bladder, the loss of bladder control that follows a head injury, also called TBI‑related bladder dysfunction, many patients also confront Neurogenic Bladder, a condition where nerves can’t properly signal the bladder to fill or empty. Understanding traumatic brain injury bladder is essential because it directly affects daily independence and quality of life. The brain‑bladder connection creates a chain reaction: the injury disrupts neural pathways, leading to urinary urgency, retention, or incontinence. This link encompasses bladder muscle overactivity and sphincter weakness, making early assessment critical for any rehab plan.
Key Factors in Managing Bladder Dysfunction After TBI
Effective bladder management requires a blend of medical, therapeutic, and lifestyle approaches. One cornerstone is Pelvic Floor Therapy, targeted exercises that strengthen muscles controlling urine flow. Strengthening these muscles can reduce urgency episodes and improve emptying efficiency. Another essential tool is scheduled voiding, which trains the bladder to empty at set intervals, reducing surprise leaks. Together, these strategies enable patients to regain control, boost confidence, and avoid the social stigma that often follows urinary accidents.
Medication plays a supporting role, especially anticholinergics that calm an overactive bladder. However, doctors must balance benefits against side effects like dry mouth or constipation, which can be problematic for someone already coping with TBI‑related fatigue. In many cases, a urologist will recommend a trial of bladder training combined with low‑dose medication to see if symptoms improve before moving to more invasive options.
Urinary Incontinence, the involuntary loss of urine is one of the most common complaints after a traumatic brain injury. It impacts not just physical health but also emotional well‑being, often leading to anxiety or depression. Recognizing that incontinence influences overall quality of life helps clinicians prioritize it alongside motor and cognitive rehab. Simple measures like absorbent pads, skin‑protecting barrier creams, and discreet clothing choices can make a huge difference while longer‑term solutions are being explored.
When conservative methods fall short, Catheterization, the insertion of a tube to drain urine directly from the bladder becomes an option. Intermittent (or clean) catheterization is usually preferred over a permanent Foley catheter because it lowers infection risk and preserves bladder sensation. Still, any catheter carries a chance of urinary tract infections, so strict hygiene protocols and regular monitoring are non‑negotiable. Health professionals often view catheter use as a temporary bridge while other therapies take effect.
Beyond medical interventions, lifestyle tweaks can ease bladder symptoms. Reducing caffeine and alcohol intake lessens bladder irritability, while staying well‑hydrated prevents concentrated urine that can irritate the lining. Weight management is also helpful; excess abdominal pressure can exacerbate leakage. Small, consistent changes add up, giving patients more control without adding medication load.
Rehab teams must also consider the timing of bladder care within the broader TBI recovery timeline. Early assessment—ideally within the first week of injury—helps map the severity of neurogenic bladder and set realistic goals. As cognitive function improves, patients become better able to follow voiding schedules and perform pelvic floor exercises. Thus, bladder management requires a dynamic plan that evolves with the patient’s overall recovery.
Family and caregivers play a pivotal role, too. Educating them about signs of urinary retention, infection, or catheter blockage can prevent complications. Caregiver support also reduces the emotional burden on the person with TBI, fostering a more collaborative environment for practicing bladder‑control techniques.
In practice, the best outcomes come from a multidisciplinary approach: neurologists, urologists, physical therapists, and occupational therapists all bring expertise that, when combined, addresses the full spectrum of bladder issues post‑TBI. This collaborative model enables personalized care plans that adapt as the patient regains function, minimizing setbacks and promoting independence.
Below you’ll find a curated list of articles that dive deeper into each of these areas— from medication guides to step‑by‑step catheter care, from pelvic floor exercise routines to coping strategies for incontinence. Whether you’re a patient, a family member, or a healthcare professional, the resources here will give you practical insights to tackle traumatic brain injury bladder challenges head‑on.

 Sep, 30 2025
Sep, 30 2025