Urinary Retention After Concussion: What You Need to Know
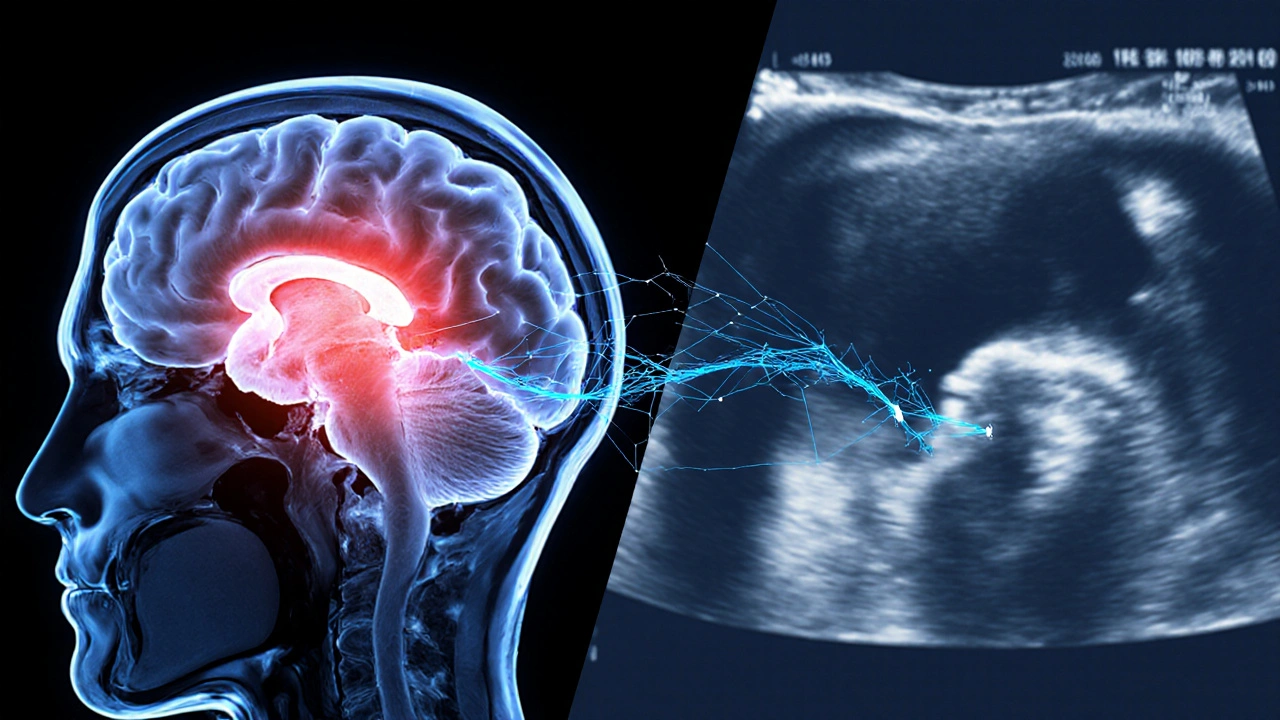
When dealing with urinary retention after concussion, the inability to empty the bladder that follows a head injury. Also known as post‑concussive urinary retention, it can feel like a sudden, frustrating block that shows up days or weeks after the impact. This condition isn’t just an annoying side effect; it signals that the nervous system’s control over the bladder may have been disrupted. The brain‑bladder connection is a two‑way street, and a concussion can throw a wrench into the signals that tell the bladder when to contract and when to relax.
Key Factors Linking Head Trauma to Bladder Trouble
First, consider concussion, a mild traumatic brain injury that alters brain function temporarily. It often brings headaches, dizziness, and cognitive fog, but the autonomic nervous system can also take a hit. autonomic dysfunction, a disturbance in the part of the nervous system that regulates involuntary actions, may develop after a concussion and affect bladder control. In plain terms, the signals that tell the bladder to empty can become scrambled, leading to urinary retention after concussion.
Another related entity is neurogenic bladder, a condition where nerve damage impairs bladder storage or emptying. After a head injury, the spinal pathways that carry messages from the brain to the sacral nerves can be compromised, creating a neurogenic component to the retention. This link forms a semantic triple: "Urinary retention after concussion encompasses neurogenic bladder dysfunction." It’s not just a coincidence; the brain injury sets off a cascade that can include weakened detrusor muscle contraction, overactive sphincter tone, or both.
Finally, the practical side of the problem often involves catheterization, the insertion of a tube to drain urine when normal voiding is impossible. While catheters can relieve immediate discomfort, they also carry risks like infection, so they’re usually a short‑term solution while the underlying neural pathways recover. Understanding why catheterization becomes necessary creates another triple: "Management of post‑concussive urinary retention often requires catheterization until nerve function stabilizes." Putting these pieces together helps you see the bigger picture. A concussion can trigger autonomic dysfunction, which in turn may produce neurogenic bladder symptoms, leading to urinary retention that sometimes needs catheter support. Knowing the chain of events lets you ask the right questions at the doctor’s office: What tests will assess nerve function? Are there medication options to smooth out sphincter tone? How long might I need a catheter, and what hygiene steps reduce infection risk? Below, you’ll find a curated collection of articles that dig deeper into each of these angles—symptom checklists, diagnostic tools, treatment pathways, and real‑world tips for coping while your nervous system heals. Whether you’re a patient, a caregiver, or a health professional, the resources will give you practical insight to manage urinary retention after concussion more confidently.

 Sep, 30 2025
Sep, 30 2025