When you start a new medication, you’re told about possible side effects. Headache. Nausea. Fatigue. Insomnia. You read the leaflet. You hear your doctor mention them. Then, within days, you start feeling them too. But here’s the twist: you might be reacting to the information-not the drug.
What Exactly Is the Nocebo Effect?
The nocebo effect isn’t imagination. It’s real. When you expect harm from a treatment-even if it’s just a sugar pill-you can develop actual physical symptoms. The word comes from Latin: nocebo means "I will harm." It’s the dark twin of the placebo effect, where positive expectations make a treatment work better. But instead of healing, nocebo makes you feel worse. In clinical trials, about 20% of people taking a placebo report side effects. Nearly 10% quit the trial because they think the treatment is making them sick. And here’s the kicker: those people weren’t given any active drug. Their bodies responded to the idea of harm. This isn’t rare. Studies show 26% to 50% of side effects reported when starting a new medication may be nocebo-driven. That means for half of the people who say a drug gave them nausea or dizziness, the drug itself might not be the cause. Their brain, shaped by warnings, past experiences, or even a doctor’s tone, created the symptoms.How Your Brain Creates Symptoms Without Drugs
Your brain doesn’t distinguish between real threats and imagined ones. When you’re told a medication might cause headaches, your brain starts scanning for any little ache. You feel a dull pressure behind your eyes? That’s the medication. You wake up tired? That’s the medication. You didn’t feel those things before-but now your brain is wired to link them to the pill. Neuroimaging studies show this isn’t just psychology. Brain areas like the anterior cingulate cortex, insula, and prefrontal cortex light up when people expect pain or side effects. These are the same regions activated during real physical pain. The brain releases stress chemicals like cortisol and activates pain pathways-even without a drug doing anything. One famous study used remifentanil, a powerful painkiller. When patients were told the drug would make them more sensitive to pain after its effects wore off, their pain levels spiked-despite still getting the same dose. When they were told it would help, the pain relief doubled. The drug didn’t change. Only the expectation did.Why Generic Drugs Trigger More Complaints
Switching from a brand-name drug to a generic version is one of the most common triggers of the nocebo effect. The active ingredient is identical. The FDA requires generics to be bioequivalent. But patients often feel worse after the switch. In New Zealand in 2017, doctors switched patients from brand-name venlafaxine to a generic version. Adverse effect reports stayed flat-for weeks. Then, media coverage aired concerns about "generic versions being less effective." Within months, reports to the national drug safety agency jumped dramatically. The drug hadn’t changed. The information had. Reddit threads are full of similar stories. One user wrote: "I switched to generic sertraline and got insomnia and nausea overnight. My pharmacist said it’s probably psychological. I felt like he was dismissing me-but he was right. When I went back to the brand, it vanished." The problem? Packaging. Pill color. Size. Taste. Even the name on the bottle. Your brain associates these cues with past experiences. If you’ve had bad side effects with one brand, your brain expects the same with any version-even if it’s chemically identical.How Doctors and Pharmacies Accidentally Cause Harm
It’s not just patients. Providers often unintentionally fuel nocebo effects. Think about how side effects are usually explained: "This drug can cause nausea, dizziness, fatigue, weight gain, anxiety, liver damage, and suicidal thoughts." That’s a long list. And it’s all true-but presented without context. Patients hear the worst-case scenarios. They don’t hear that nausea affects 5% of people, or that liver damage is rarer than being struck by lightning. A 2021 European study found 68% of physicians admit they’ve seen patients develop symptoms after being warned about them. That’s not malpractice. It’s poor communication. The fix isn’t to hide risks. It’s to reframe them. Instead of saying, "Some people get severe headaches," say, "Most people take this without any issues. A small number might feel a mild headache the first week-it usually goes away. If it doesn’t, we’ll adjust." In New Zealand, training doctors in this kind of communication cut medication discontinuation rates by 18%. That’s not magic. It’s science.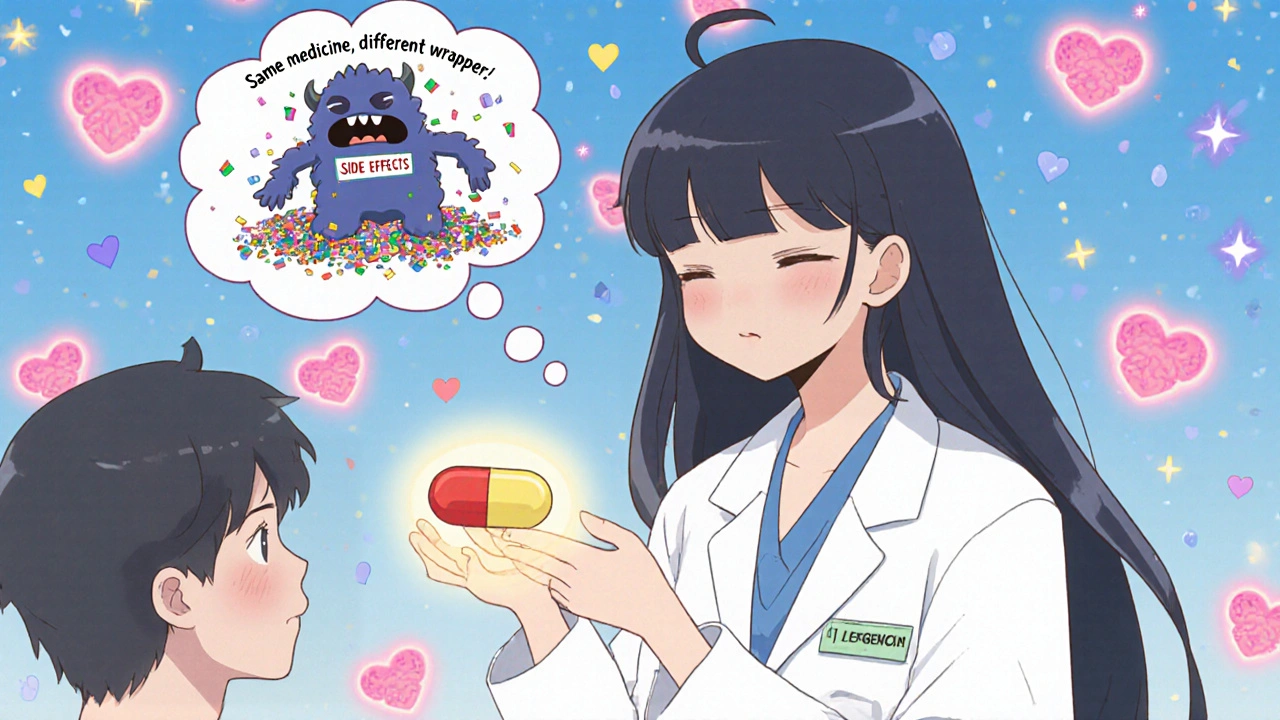
Who’s Most at Risk?
Not everyone is equally affected. Certain people are more vulnerable to the nocebo effect:- Women-report 23% more side effects than men in placebo groups
- People with anxiety or depression-1.7 times more likely to experience nocebo symptoms
- Those who’ve had bad reactions to meds before
- People who read medication leaflets cover to cover
- Those who search online for side effects before even starting a drug
What You Can Do to Protect Yourself
If you’re starting a new medication, here’s what actually helps:- Don’t read the leaflet before taking the drug. Wait until after you’ve started. You’ll know what’s real and what’s imagined.
- Ask your doctor: "What’s the most common side effect, and how often does it happen?" Avoid the fear list. Focus on likelihood.
- Track symptoms objectively. Use a simple journal: "Day 3: mild headache, lasted 2 hours, no nausea." This separates real patterns from anxiety.
- If you feel worse after switching to generic, wait 2 weeks. Your brain might be adjusting to the new pill shape or color-not the drug.
- Don’t assume every new ache is the medication. Stress, sleep loss, or a cold can mimic side effects.
Why This Matters Beyond Your Prescription
The nocebo effect isn’t just about individual discomfort. It’s a public health issue. People stop taking life-saving medications because they think they’re causing side effects. Blood pressure pills. Antidepressants. Cholesterol drugs. All are abandoned at alarming rates-often due to nocebo, not pharmacology. Pharmaceutical companies lose billions. Health systems waste money on unnecessary tests and doctor visits. Patients suffer from untreated conditions because they stopped the one thing that could help. The World Health Organization now lists "reducing nocebo effects" as a key goal in its Medication Without Harm initiative. The FDA and European Medicines Agency are rewriting patient information guidelines to avoid fear-based language. This isn’t about hiding risks. It’s about delivering them in a way that doesn’t trigger harm.Future of Medication Communication
By 2030, experts predict doctors will routinely screen for nocebo risk before prescribing. Think of it like checking for allergies-but for expectations. Some hospitals are already testing "open-label placebos"-giving patients sugar pills but telling them honestly: "This is inert, but studies show it can still help your body heal through expectation." It sounds crazy. But in trials, it’s working for chronic pain, IBS, and fatigue. The future of medicine isn’t just better drugs. It’s smarter communication. It’s understanding that your brain is part of the treatment.Frequently Asked Questions
Can the nocebo effect cause real physical damage?
Yes, but not in the way most people think. The nocebo effect doesn’t cause organ damage or disease progression. Instead, it triggers real physiological changes-like increased stress hormones, muscle tension, or altered pain signaling-that feel like side effects. These are temporary and reversible. They don’t cause long-term harm, but they can make you feel so unwell that you stop taking necessary medication, which can lead to real health risks.
Is the nocebo effect the same as hypochondria?
No. Hypochondria involves persistent fear of having a serious illness despite medical reassurance. The nocebo effect is a specific response to treatment expectations. You don’t need to be anxious overall to experience it. Even someone with no history of health anxiety can develop side effects after being told a drug might cause them. It’s about context, not personality.
Why do some people feel worse on generics even when they’re identical?
It’s not about the chemistry. It’s about perception. Pills vary in color, size, shape, and even the inactive ingredients (like dyes or fillers). Your brain links these cues to past experiences. If your previous brand caused nausea, your brain expects the same from any pill that looks different-even if it’s chemically identical. Media reports and pharmacist warnings can also trigger this response. The drug works the same; your expectation doesn’t.
Can doctors legally avoid telling me about side effects to prevent nocebo?
No. Informed consent requires disclosure of known risks. But how they communicate those risks matters. Doctors can and should avoid overwhelming patients with a long list of rare or extreme side effects. Instead, they can say: "Most people tolerate this well. The most common side effect is mild nausea, which affects about 1 in 10 people and usually fades in a week. If you feel worse, we can adjust. But don’t assume every new feeling is from the drug." This is still honest-it’s just smarter.
Are nocebo effects only about pills?
No. The nocebo effect applies to any medical treatment. You can experience it with injections, surgeries, physical therapy, or even dietary changes. If you’re told a procedure might be painful, you’ll feel more pain-even if the actual stimulus is the same. It’s not about the treatment. It’s about what your brain believes it will do.

 Nov, 30 2025
Nov, 30 2025

Kelly Essenpreis
November 30, 2025 AT 19:39Alexander Williams
December 2, 2025 AT 00:53Suzanne Mollaneda Padin
December 3, 2025 AT 22:24Erin Nemo
December 4, 2025 AT 21:44ariel nicholas
December 6, 2025 AT 07:43Rachel Stanton
December 6, 2025 AT 16:52Amber-Lynn Quinata
December 7, 2025 AT 12:19Lauryn Smith
December 8, 2025 AT 18:49Bonnie Youn
December 10, 2025 AT 11:05Edward Hyde
December 11, 2025 AT 11:38Charlotte Collins
December 12, 2025 AT 01:26Margaret Stearns
December 12, 2025 AT 11:40amit kuamr
December 12, 2025 AT 13:55