Switching from brand-name Coumadin to a generic version of warfarin sounds simple-cheaper, same active ingredient, FDA-approved. But for patients on warfarin, that switch isn’t just a pharmacy change. It’s a potential trigger for dangerous blood clots or life-threatening bleeding. Why? Because warfarin has a narrow therapeutic index. That means the difference between a safe dose and a dangerous one is tiny. Your INR (International Normalized Ratio) must stay between 2.0 and 3.0 for most people. Go above 4.0? Risk of bleeding skyrockets. Drop below 1.5? Clots can form. And when you switch between generic brands, even tiny differences in how the drug is absorbed can push that number out of range.
Why Warfarin Is Different From Other Medications
Most drugs have a wide safety margin. Take ibuprofen: 200 mg, 400 mg, 600 mg-it’s hard to overdose accidentally. Warfarin isn’t like that. A 1 mg change in dose can swing your INR by 0.5 or more. That’s why doctors don’t just write a prescription and walk away. They check your INR regularly-sometimes weekly, sometimes daily-until your numbers stabilize. The problem with generic switching isn’t that generics are unsafe. They’re not. The FDA requires them to be bioequivalent to Coumadin: meaning they deliver the same amount of drug into your bloodstream within an 80-125% range. But for warfarin, that 45% window is too wide. Two generics can both meet FDA standards and still cause your INR to jump or drop when you switch between them. Studies show this isn’t theoretical. In a 2000 study of 182 patients in a St. Louis HMO, switching from Coumadin to a specific generic (Barr Labs) showed no major changes in INR control. But that was one generic, one manufacturer. When patients switched between different generic brands-say, from Teva to Mylan to Sandoz-the risk of INR fluctuations went up. One patient might handle it fine. Another might bleed internally a week later because their INR jumped to 5.2.What Happens When You Switch Generics
If you’ve been stable on Coumadin for years, your doctor might not think twice about switching you to a cheaper generic. But here’s what often gets missed: you’re not switching from brand to generic-you’re switching from one generic to another generic. That’s the real risk. In a 2021 review of 11 studies involving over 40,000 patients, researchers found that while most patients had no issues, a small but significant number had INR changes of more than 0.5 units after switching. That might not sound like much-but in warfarin terms, it’s enough to cross into danger zones. One study showed that 15-20% of patients needed more frequent INR checks in the first month after switching. A few needed emergency treatment. The Cleveland Clinic’s anticoagulation team tracks this closely. They report that 80% of patients transition smoothly. But for the other 1 in 5, it’s not smooth at all. One patient switched from Teva to Mylan warfarin and ended up in the ER with a subdural hematoma. Her INR had climbed to 6.8. No new medications. No dietary changes. Just a pharmacy refill from a different manufacturer.When and How to Monitor After a Switch
If you’re switching warfarin brands-whether from Coumadin to generic, or one generic to another-you need to treat it like starting the drug for the first time. Here’s what the guidelines say:- Check your INR within 3 to 5 days after the switch.
- Check again in 5 to 7 days.
- If both readings are stable, check weekly for the next 2 weeks.
- Only return to your normal schedule (every 4-6 weeks) if your INR stays in range for at least two consecutive checks.
What to Do If Your INR Changes After a Switch
If your INR is too high (say, 4.5 or higher), you might need vitamin K, or even a blood transfusion in severe cases. Too low (1.2 or below)? You’re at risk for stroke or pulmonary embolism. The standard adjustment is a 5-10% change in your daily dose. If you take 5 mg a day and your INR dropped from 2.8 to 2.0, you might increase to 5.5 mg. If it jumped to 4.0, you might drop to 4.5 mg. But this isn’t guesswork. Your provider should use a dosing algorithm or a clinical decision tool-not just eyeball it. Keep a log. Write down your dose, your INR, and the manufacturer name of the pill you took. If your INR goes off track, that log becomes critical. Was it the Teva pill? The Mylan one? The bottle says “warfarin sodium 5 mg”-but the manufacturer matters. The Institute for Safe Medication Practices recommends writing the manufacturer name on your medication log. Don’t just trust the pharmacy label.Why DOACs Are Changing the Game
Newer anticoagulants-apixaban, rivaroxaban, dabigatran-don’t need INR checks. They’re called DOACs (direct oral anticoagulants). They’re more expensive-$300 to $500 a month-but they’re safer for many people because they don’t interact with food or most drugs. Their bleeding risk is lower, and they don’t require constant monitoring. That’s why DOACs now make up about 65% of new anticoagulant prescriptions. But warfarin isn’t disappearing. It’s still the only option for people with mechanical heart valves. It’s still the go-to for patients with severe kidney failure. And for millions on Medicare, it’s the only affordable option. Generic warfarin costs $4 to $10 a month. DOACs cost 50 times more. So if you’re on warfarin because of cost, you’re not alone. About 1.2 million Medicare beneficiaries still use it. And for them, generic switching isn’t a convenience-it’s a necessity. But that doesn’t mean safety should be sacrificed.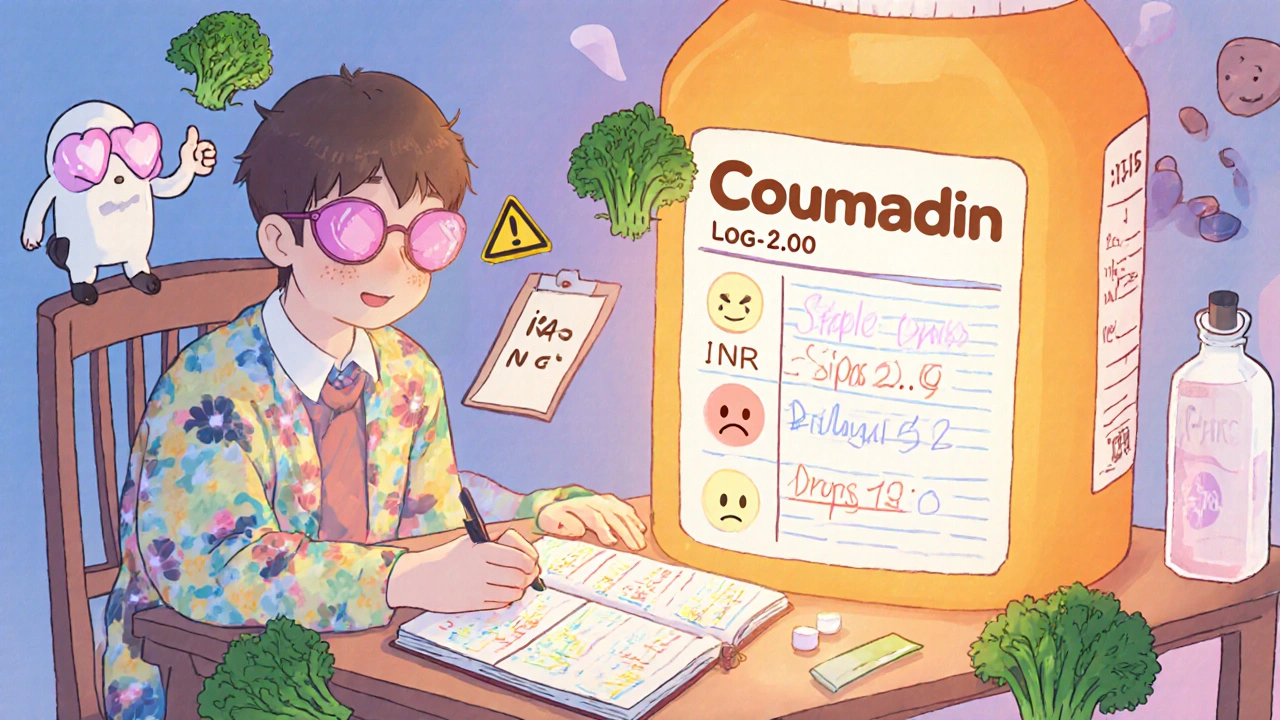
What Patients Can Do to Stay Safe
You don’t need to be a doctor to protect yourself. Here’s what you can do:- Always ask your pharmacist: “Is this the same brand I got last time?” If they say “yes,” ask for the manufacturer name. Write it down.
- Keep a calendar of your INR checks. Mark the date you switched pills.
- If you get a new prescription and the pill looks different-color, shape, markings-ask why. Don’t assume it’s the same.
- Don’t skip your INR checks, especially after a switch.
- Report any unusual bruising, bleeding gums, dark stools, or headaches to your doctor immediately.
The Bottom Line
Generic warfarin is safe-when it’s managed right. But switching between brands, even FDA-approved ones, carries risk. The data is clear: some patients handle it fine. Others don’t. And there’s no way to know who’s who until it’s too late. The solution isn’t to ban generics. It’s to treat every switch like a new prescription. Monitor closely. Document everything. Communicate with your care team. And if you’re on warfarin, never assume “same drug” means “same effect.” The FDA says all warfarin products are therapeutically equivalent. But the real world doesn’t always follow the lab results. Your body is the final test. And your INR? That’s the only number that matters.Can I switch between different generic warfarin brands without checking my INR?
No. Even though all generic warfarin products are FDA-approved as equivalent, switching between different manufacturers can cause your INR to rise or fall unexpectedly. Always check your INR within 3-5 days after switching, then again in 5-7 days. Continue weekly checks for two weeks to ensure stability.
Why does warfarin need more monitoring than other blood thinners?
Warfarin has a very narrow therapeutic index-meaning the difference between a safe dose and a dangerous one is small. It’s also affected by diet (especially vitamin K), other medications, alcohol, and even changes in your liver function. Newer blood thinners (DOACs) don’t interact with food or most drugs and don’t require regular blood tests.
Is generic warfarin less effective than Coumadin?
No. Generic warfarin is just as effective as Coumadin when taken correctly. The issue isn’t effectiveness-it’s consistency. Small differences in how the body absorbs the drug from different manufacturers can cause your INR to fluctuate. That’s why monitoring after a switch is critical.
What should I do if my INR suddenly changes after switching generics?
Don’t adjust your dose yourself. Contact your doctor immediately. They may order a repeat INR, check for other causes (like new medications or diet changes), and adjust your dose by 5-10% based on your results. If your INR is very high (above 5.0), you may need vitamin K or urgent medical care.
Should I ask my doctor to keep me on Coumadin instead of generics?
If you’re stable on Coumadin and can afford it, staying on it avoids the risk of switching. But if cost is an issue, generics are safe if monitored properly. Ask your doctor to document your current brand and manufacturer in your records, and request extra INR checks for the first month after any switch.
Next Steps for Patients on Warfarin
If you’re on warfarin right now, here’s what to do next:- Check your last INR result and the date of your last refill. Did you switch brands recently?
- Look at your pill. Does it look different from last month? Check the imprint code (the letters/numbers on the pill) and compare it to your previous bottle.
- Call your pharmacy and ask: “What manufacturer made my last warfarin prescription?” Write it down.
- Call your doctor’s office. Ask: “Do I need an INR check after my last switch?” If they say no, ask why-and insist on one if you’re unsure.
- Keep a simple log: Date, Dose, Manufacturer, INR Result. Bring it to every appointment.

 Nov, 17 2025
Nov, 17 2025

Conor McNamara
November 18, 2025 AT 23:26so i switched to generic warfarin last month and my INR went from 2.4 to 4.9 in 3 days… no new meds, no kale smoothies, just a different pill. now i’m scared to even swallow anything. the pharmacist said it’s ‘therapeutically equivalent’ like that’s some kind of magic spell. i think they’re all the same but my body knows better. i’m not taking another pill until i get a blood test. and i’m writing the manufacturer on my arm now. just in case.
Leilani O'Neill
November 20, 2025 AT 14:04It’s absurd that we allow this. The FDA’s 80-125% bioequivalence window is a joke when you’re talking about a drug that can kill you with a 1mg shift. This isn’t aspirin. This isn’t ibuprofen. This is a precision instrument, and we’re letting pharmacists play Russian roulette with people’s lives. The system is broken, and the only reason it still functions is because patients are too exhausted to fight back.
Riohlo (Or Rio) Marie
November 21, 2025 AT 18:18Oh honey, let me tell you about my cousin’s friend who switched from Teva to Mylan and ended up with a subdural hematoma. She didn’t even know she’d been switched. The pharmacy didn’t tell her. The doctor didn’t check. The INR was 6.8. They had to give her vitamin K like it was a damn cocktail. And now? She walks with a cane. And the insurance company? They sent her a coupon for a $5 generic. That’s the American healthcare system. A tragedy wrapped in a discount sticker.
steffi walsh
November 23, 2025 AT 16:59Hey everyone, I just wanted to say you’re not alone. I’ve been on warfarin for 7 years and I keep a little notebook with the pill colors, numbers, and manufacturer. It’s my peace of mind. I check my INR every week after a switch, no matter what anyone says. You’re doing the right thing by paying attention. Keep going. You’re stronger than you think.
Shilpi Tiwari
November 24, 2025 AT 13:26From a clinical pharmacology perspective, the pharmacokinetic variability in warfarin enantiomers (S- and R-) across generic formulations is non-trivial due to differences in excipient composition affecting dissolution kinetics. The CYP2C9 and VKORC1 polymorphisms further modulate this, rendering population-level bioequivalence metrics insufficient for individual risk stratification. Hence, the 3-5 day INR protocol is not merely prudent-it’s pharmacodynamically imperative.
Christine Eslinger
November 26, 2025 AT 05:17I’ve been a nurse for 22 years and I still get chills reading stories like this. The worst part? It’s preventable. Every single time someone switches, they should get an INR within 72 hours. Period. No excuses. I’ve seen people die because someone thought ‘it’s just a generic.’ It’s not. It’s your life. Please, if you’re on warfarin-track your pills. Ask questions. Demand checks. You deserve to be safe.
Denny Sucipto
November 26, 2025 AT 14:23Man, I used to think generics were just cheaper stuff. Then my dad had a stroke after switching warfarin brands. He didn’t even know he was switched. Now I check every bottle like it’s a bomb. I write the maker on the pill bottle with a Sharpie. I know it sounds crazy-but I’d rather look like a weirdo than bury my dad again.
Holly Powell
November 28, 2025 AT 03:19It’s fascinating how the medical community clings to outdated protocols while ignoring the data. The 2021 meta-analysis showed a 15-20% incidence of INR shifts post-switch-yet primary care physicians still default to ‘it’s fine.’ This isn’t negligence; it’s systemic epistemic failure. The FDA’s equivalence standard is a relic of 1980s regulatory pragmatism, not modern pharmacology. We need biomarker-guided switching protocols. Not guesswork.
Emanuel Jalba
November 29, 2025 AT 16:00THIS IS WHY I HATE BIG PHARMA AND THE GOVERNMENT 😭🩸💀 I’m on warfarin and I’ve had 3 near-death experiences because of generic switches. I’ve cried in the ER. I’ve screamed at my doctor. I’ve Googled ‘can warfarin kill you’ at 3am. And now I have to write the manufacturer on my fridge? My life is a pharmacy lottery. I just want to live. I’m not asking for much. Just don’t switch my pills without warning me. Please.
Heidi R
November 30, 2025 AT 01:25You’re all overreacting. The data shows 80% transition smoothly. The other 20%? Probably noncompliant or had other risk factors. Stop being dramatic. Just check your INR and move on.
Brenda Kuter
November 30, 2025 AT 06:01They’re lying to us. I know it. The FDA, the pharmacies, the doctors-they all get kickbacks from the generic manufacturers. That’s why they say it’s safe. My cousin’s husband died after a switch. They buried him in a cheap coffin. And now they want me to trust a pill that looks different? I won’t. I’m switching to DOACs. Even if I have to sell my car. I’m not dying because of a cost-cutting scheme.
Shaun Barratt
November 30, 2025 AT 18:12Per the American College of Chest Physicians guidelines (2021), the recommended INR monitoring protocol following a generic substitution is unequivocal: serial measurements at 3–5 days and 5–7 days post-switch, followed by weekly assessments until two consecutive stable values are obtained. Deviation from this protocol constitutes a breach of the standard of care. Documentation of manufacturer, batch number, and INR trajectory is not merely advisable-it is a medico-legal imperative.
Iska Ede
December 2, 2025 AT 07:21Wow. So the solution to a $4 pill is to turn every patient into a full-time lab technician? Congrats, you just invented the world’s most stressful hobby. Next you’ll want us to calibrate our own INR machines with a paperclip and a prayer. Meanwhile, DOACs are $500/month. So thanks, capitalism. You win again.